Resources
Style
Planning
View All
THE blog
Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Your menstrual cycle isn’t just about fertility—it’s a vital sign of your overall health. A healthy cycle is often an indicator of wellness, while irregularities can be a red flag for potential health issues. Just like your heart rate, blood pressure, and respiratory rate, your cycle provides valuable insights into your body’s well-being. Understanding and tracking it can help you detect potential health problems early and take proactive steps toward better health. Whether you’re looking to optimize your health or manage a condition, your menstrual cycle is a powerful tool for self-awareness. Let’s dive into why your menstrual cycle is the ultimate monthly report card for your body.
Why Your Menstrual Cycle Matters
Ovulation is more than just a reproductive function—it’s a key indicator of your overall health. A regular menstrual cycle means your body is producing hormones in a balanced way, supporting everything from bone density to cardiovascular health. When your cycle is off, it might be your body’s way of signaling an underlying issue like hormonal imbalances, nutrient deficiencies, or even chronic conditions such as polycystic ovary syndrome (PCOS) or thyroid disorders.
The Menstrual Cycle as a Vital Sign
Medical professionals now recognize the menstrual cycle as the “fifth vital sign” because it reflects overall physiological health. A healthy cycle indicates that your hormones are functioning properly, while irregularities could signal potential concerns such as:
- Hormonal imbalances – Irregular periods can be a sign of PCOS, thyroid dysfunction, or estrogen dominance.
- Nutritional deficiencies – A lack of key nutrients like iron, zinc, and vitamin D can affect your cycle’s regularity and flow.
- Stress and lifestyle factors – High stress, poor sleep, or over-exercising can impact ovulation and menstrual health.
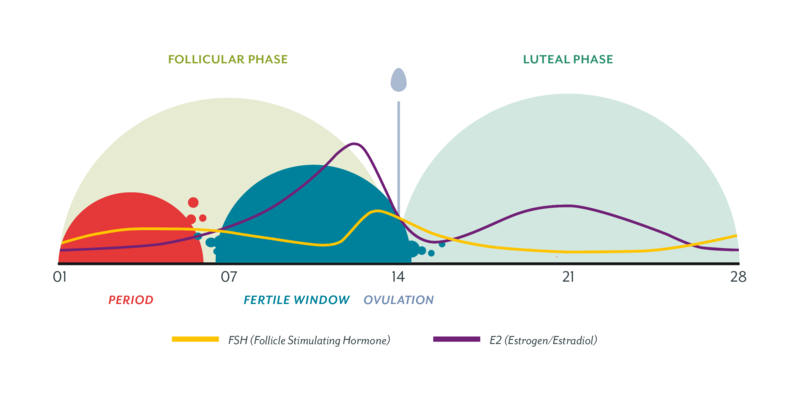
The Phases of the Menstrual Cycle
Understanding the four phases of the menstrual cycle can help you align your lifestyle, nutrition, and self-care routines with your body’s natural rhythm.
- Menstrual Phase (1-6 days)
- This phase begins with the shedding of the uterine lining.
- Energy levels may be low, and the body benefits from rest and nutrient-dense foods.
- Follicular Phase (7-21 days)
- The body starts preparing for ovulation by increasing estrogen production.
- This is an optimal time for creativity, social activities, and higher-intensity workouts.
- Ovulatory Phase (1 day)
- The body releases an egg, and estrogen peaks.
- Many women experience increased energy, confidence, and libido during this time.
- Luteal Phase (10-16 days)
- Progesterone rises, preparing the body for a potential pregnancy.
- PMS symptoms may appear, and the body may crave more rest and nourishing foods.
Aligning your activities with these phases can help you optimize performance, reduce stress, and support hormonal balance. Learn more about eating for your cycle here.
What a Healthy Menstrual Cycle Looks Like
A normal menstrual cycle varies from person to person, but generally:
- Cycle length: 21–35 days (consistently within an 8-day range)
- Menstruation duration: 3–7 days with a blood loss of about 25–80 mL
- Ovulation: Occurs between days 10–23, followed by a luteal phase of 12–14 days
- Cervical mucus changes: 2–7 days of cervical mucus with at least one day of peak mucus before ovulation
If your cycle frequently falls outside these parameters, it might be time to investigate further.
What Your Menstrual Cycle Can Reveal About Your Health
Your menstrual cycle is an important indicator of your overall health, and any changes or irregularities can signal underlying issues. Here are some signs to watch for:
- No cycle: This could indicate anovulation, amenorrhea, stress or trauma, or possibly PCOS.
- Skipped cycles: Anovulation, stress or trauma, or potentially PCOS.
- Cycles longer than 35 days: Anovulation or PCOS.
- Cycles shorter than 21 days: May point to a luteal phase defect (and see “Luteal Phase shorter than 10 days”).
- Luteal phase shorter than 10 days: Low progesterone due to inadequate follicle or corpus luteum development, which may be linked to egg quality issues, inflammation, thyroid dysfunction, insulin metabolism problems, or nutrient deficiencies (especially magnesium, B vitamins, Vitamin D, iodine, zinc, selenium).
- Heavy flow: This can indicate estrogen dominance, often accompanied by painful cramps, tender breasts, headaches, fluid retention, and mood swings.
- Light flow/Dark or brown color: This could suggest inadequate corpus luteum development or uterine lining thickening, with low estrogen, FSH, or LH levels.
- Menstrual fluid odor: A possible sign of infection or dysbiosis.
- Cramping: Often associated with estrogen dominance.
- Bleeding outside of menstruation: Spotting in the luteal phase could indicate low progesterone production, often due to issues with follicular or corpus luteum development.
- Vaginal discharge/cervical mucus changes: Typically, the pattern will progress from dry → sticky → creamy → egg white → sticky → dry.
If any of these signs are present, it may be time to seek medical advice and investigate further.
Learn more about how optimizing gut health can help manage PCOS here: Understanding PCOS and Gut Health
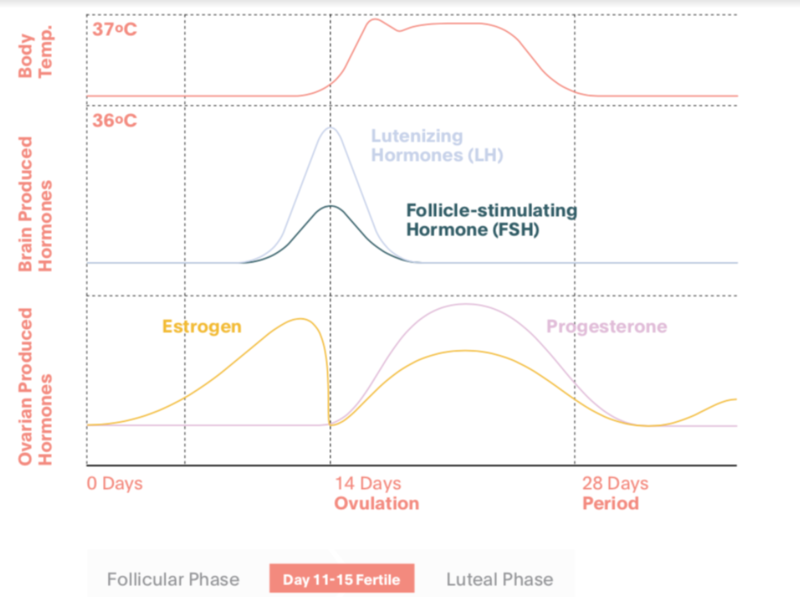
How Hormones Influence Your Cycle
Two primary hormones drive the menstrual cycle: estrogen and progesterone.
- Estrogen helps build up the uterine lining and triggers the release of an egg during ovulation.
- Progesterone stabilizes the uterine lining, supports pregnancy, and helps balance estrogen’s effects.
When these hormones are out of balance, it can lead to irregular periods, mood swings, fatigue, and other symptoms. Proper ovulation is essential not just for fertility but for long-term health, as it helps protect against conditions like osteoporosis, cardiovascular disease, and even certain cancers.
Natural Ways to Balance Female Sex Hormones
Balancing hormones naturally can improve menstrual health and overall well-being. Here are key strategies to support hormone balance:
- Nutrient-Dense Diet – Prioritize whole foods rich in fiber, healthy fats, and essential vitamins. Foods like leafy greens, cruciferous vegetables, and omega-3 fatty acids help regulate estrogen levels.
- Gut Health Support – A healthy gut microbiome plays a crucial role in hormone metabolism. Probiotic-rich foods like yogurt, kefir, and fermented vegetables can aid digestion and hormone balance.
- Reducing Toxins – Environmental toxins found in the 4 P’s (plastics, pesticides, pollution and personal care products) can act as endocrine disruptors. Switching to natural alternatives can help minimize exposure to hormone-disrupting chemicals.
- Stress Management – Chronic stress increases cortisol levels, which can disrupt estrogen and progesterone balance. Practices like meditation, deep breathing, and regular movement can help lower stress levels.
- Common causes of stress:
- Chronic stressors → oxidative stress, inflammation, immune dysfunction, thyroid suppression (“rest and repair”)
- Common causes of stress:
- Sleep Optimization – Aim for 7-9 hours of quality sleep each night, as inadequate rest can negatively impact hormone regulation.
- Sleep signs that indicate something is “off”:
- Light sleeping/lack of deep sleep → low progesterone
- Waking frequently to urinate → sign of chronic stress
- Waking between 1-3am, night sweats → liver detoxification
- Sleep signs that indicate something is “off”:
Tracking Your Cycle: A Powerful Health Tool
Charting your cycle helps you understand your body’s unique rhythm and detect early signs of imbalance. Fertility awareness methods (FAM) focus on tracking:
- Basal body temperature (BBT) – A rise in temperature indicates ovulation has occurred.
- Cervical mucus patterns – Clear, stretchy mucus signals peak fertility.
- Cervical position – Changes throughout the cycle, helping identify fertility windows.
Tracking these signs can give you a clearer picture of your health, help you time conception (or avoid pregnancy naturally), and even provide clues about underlying health issues.
Lifestyle and Nutrition for a Healthy Cycle
Supporting your menstrual health involves more than just tracking—it’s about optimizing your lifestyle:
- Eat nutrient-dense foods: Include healthy fats, iron-rich foods, and plenty of fiber.
- Manage stress: High cortisol levels can disrupt ovulation.
- Get enough sleep: Poor sleep affects hormone production.
- Exercise wisely: Overtraining can negatively impact your cycle, while moderate movement supports hormone balance.
The Pill and Menstrual Health
Hormonal contraceptives suppress ovulation, meaning they override your body’s natural cycle. While effective for pregnancy prevention, long-term use can deplete essential nutrients like folate, vitamin B6, and zinc. Research also shows that hormonal contraceptives can impact cervical health, making women up to 85% less likely to clear HPV infections, which increases the risk of cervical cancer. Additionally, long-term pill use has been linked to folate deficiency, affecting cell repair and increasing the chances of abnormal cervical changes. Nutritional support, including adequate folate, vitamin A, and B vitamins, may help mitigate some of these effects. Understanding these potential impacts can help individuals make informed decisions about their contraceptive choices.
Learn more about the steps to take before getting off hormonal birth control here.
Take Charge of Your Cycle
Your menstrual cycle is a powerful health indicator that deserves attention. By tracking and understanding your cycle, you gain insights into your body’s needs, allowing you to make informed decisions about your health. If you notice irregularities, don’t ignore them—your cycle is your body’s way of communicating with you.
Want to start tracking? Use a simple journal, an app, or work with a fertility nutritionist to get a deeper understanding of your unique cycle. Your period isn’t just a monthly inconvenience—it’s a crucial barometer of your health!

Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC7643763
https://drbrighten.com/stopping-birth-control-side-effects
One of the best ways to start prepping for pregnancy and optimizing your fertility, is to become more aware of your sex hormones like estrogen, progesterone, and testosterone. If you’ve been tracking your cycle for a while now, you may know that there are two distinct phases of the cycle – your follicular phase and your luteal phase.
Many women experience issues in their luteal phase, which is connected to the hormone progesterone. In this blog, we’ll cover in depth what progesterone is, how to measure it, and what you can do to improve progesterone levels naturally.

What is Progesterone?
Progesterone is a steroid hormone made from cholesterol, and is made from luteine cells in the uterus. These cells will make progesterone until the placenta is strong enough to make progesterone on it’s own, and will continue to do so for the rest of pregnancy.
We make progesterone for about 2 weeks during the luteal phase after ovulation.
The follicle turns into the corpus luteum (aka yellow body), which is what makes progesterone. Your body does not make progesterone in the first half of your cycle.
The first half of your cycle (your follicular phase) is where estrogen is released. You need that rise in estrogen to ovulate, and then progesterone kicks in.
So why is this important for fertility?
Progesterone is your pro-gestation hormone. It helps grow a baby in your uterus and thrive there. When progesterone is made, it’s made for the first 8-10 weeks from the corpus luteum, at which point the placenta should be strong enough to take over.
However, for some women their corpous luteum is not strong enough to make progesterone last for 8-10 weeks, which often leads to early pregnancy loss. Having a healthy amount of progesterone plays a large factor in preventing miscarriage.
The problem is, many fertility clinics will test progesterone from a blood draw on one day of the cycle, but the levels of progesterone can change dramatically throughout the day (and month). Additionally, many women don’t know that they need to check their progesterone levels in the second half of the cycle – this is KEY!
One way to check progesterone levels at home is by using progesterone test strips, like the Proov test strips – which will tell you if you have healthy levels of progesterone after ovulation.
In addition to helping to prevent miscarriage, progesterone is important for priming the uterine lining for implantation.
When should levels be measured for progesterone?
If you’re working with a fertility clinic, it’s important that you check your progesterone levels in the second half of your cycle. Remember, you don’t make progesterone in the first half of your cycle.
Ideally, you would check progesterone levels 5-7 days after ovulation. If you ovulate on day 14, then you want it on day 19-21 to measure, before the start of your period.
While a serum test can be helpful, a DUTCH test provides more information because it measures progesterone at 4 different points throughout the day and takes the average.
[If you’re interested in taking the DUTCH test and having your labs interpreted by me, schedule a call below to chat!]

Because progesterone will be vastly different at different times of the day, it’s best to get a reading at different parts of the day for the most accurate picture of your progesterone levels.
Additionally, progesterone can be made on certain days but then can putter out very quickly. Some signs of low progesterone could be tender breasts, PMS symptoms, and heavy periods.
What are Optimum Serum Levels of Progesterone?
Ideally, serum levels are above 10. Lower numbers are indicative of a weak corpus luteum, and if your levels are extremely low, it could be that you’re not ovulating at all, and rather progesterone is being made from the adrenals glands, and not the ovaries at all.
SIGNS OF LOW PROGESTERONE:
- PMS – mood changes, bloating, tender breasts
- Heavy periods, clotting, worse endometriosis symptoms
- Insomnia and stress or anxiety before period (progesterone impacts GABA, a neurotransmitter that calms things down)
- Spotting before period (losing the uterine lining that you’re supposed to maintain)
- Short luteal phase (should be 12-14 days ideally, anything shorter can be a sign of low progesterone)
Suggested Reading: How to Find Your Fertile Window
Remember, hormones are not just about reproduction – hormones impact the cardiovascular system, brain health, immune system, gut health, and essentially every system in the body!
What You Can Do to Increase Progesterone
Okay, so now that we know progesterone is important, and perhaps you’ve noticed signs of low progesterone either from a test, or symptoms mentioned above – what can you do about it?

1. Manage your stress levels
When you have a lot of stress, whether or not it’s real stress or perceived stress – your body will react in the same way.
Cortisol, epinephrine and norepinephrine will feed back to the brain and let your brain know that there’s a lot of stress here.
The brain will then decrease signaling of estrogen and progesterone. Women will first lose progesterone, which will cause you to not ovulate. If the stress is strong enough, then it will down regulate FSH and estrogen, and you will have amenorrhea and skip cycles completely.
This is your body’s way of protecting you. If you’re being chased by a tiger (stress), it’s probably not a good time to make a baby. So working on self care, and anything to support your body like good sleep, healthy relationships, regular movement, etc. is going to be helpful in managing stress, but also in making enough progesterone.
Of course, if you’re trying to conceive or in the middle of fertility treatments, you’re likely very stressed. It’s not helpful for me to tell you that you just need to stop stressing, but understanding the biochemistry behind how stress impacts ovulation and progesterone can give you a better understanding of how your lifestyle choices are impacting fertility.

2. Work on Your Gut Health
Your immune system starts in the gut, and any inflammation happening there will negatively impact progesterone production as well.
Whether you are taking a comprehensive stool test, or just taking the 5R approach to gut health – taking care of your digestion will help balance out your hormones in the long run.

3. Stop Under-Eating and Over-Exercising
As a reminder, all steroid hormones are made from cholesterol. If you have very low levels of cholesterol you may be not be able to make sex hormones like estrogen and progesterone.
Additionally, leptin (a hormone made from fat tissue) is a big sign for fertility -it will tell your brain if you have enough fat on you to actually carry a pregnancy term.
If you’re a marathon runner, extreme athlete, have an active eating disorder, or just really cutting calories and over-excerising and have a very low body fat percentage, your cycles will stop or skip in order for your body to reduce your chances of getting pregnant.
HOW TO BALANCE PROGESTERONE THROUGHOUT THE CYCLE
If you’re having troubles with your progesterone levels or have a short luteal phase, it may be tempting to JUST focus on the second half of your cycle.
The truth is that you need to support your cycle all month long to help with luteal phase defects.
In the follicular phase, your brain makes FSH to make estrogen. One follicle is chosen to release an egg, and you need to have estrogen elevated for 40-50 hours, to get an LH surge which triggers ovulation, which is what triggers corpus luteum, which triggers progesterone production.
You can’t just focus on progesterone, because there is a domino effect between all of these hormones.
Low progesterone is also a sign of low follicular health or poor egg quality. Giving progesterone as a medication does not address the root problem. While there is no adverse effect of taking progesterone, working on diet and lifestyle changes will benefit you in the long run.
That’s why working on your hormone health for at least 3 months before conceiving will be important in order to work on egg quality, progesterone, and address the root cause issues.
Natural Therapies to Increase Progesterone Levels
- Supplements that Help with Brain Health: Omega 3 fats, Gingko, Rosemary, Maca, Cordyceps – are all great for brain health. We want good signaling from the brain to the ovaries (HPO axis) Trying to get the brain back on track with neuron signaling. Maca, Cordyceps, Lion’s Mane (great for focus), and Chaga medicinal mushrooms.
- Antioxidants play a huge role on the ovaries. Melatonin, lutein foods like beta-carotene, vitamin C, selenium, and zinc can be extremely helpful to the ovaries.
- Vitex / Chaste Tree is a very common herb used to improve both estrogen and progesterone levels. Vitex has been shown to increase LH, and subsequent progesterone levels in women with luteal phase defects. This herb is not necessarily fast acting, but taken every day for 3 months has shown improvements in women in several studies.
Looking for More?
If you’re looking for more support, functional lab testing, and nutrition counseling to help you conceive, let’s schedule a free 30 minute discovery call!

I work with women in their 20s, 30s, and 40s trying to conceive – whether you have PCOS, endometriosis, or unexplained infertility, we will work together to get to the root issue and improve your chances of becoming pregnant.
I hope you learned something from this blog post, and let me know what questions you have below!
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook
