Nutrition
Resources
Style
Planning
View All
If you’ve been diagnosed with Polycystic Ovary Syndrome (PCOS), you’ve probably been told that birth control is the go-to solution. While it can help regulate cycles and manage symptoms, it’s not a one-size-fits-all fix—and it certainly doesn’t address the root causes of PCOS. The good news? There are plenty of science-backed, natural strategies to help you take control of your health, balance your hormones, and feel your best. From nutrition and exercise to stress management and supplements, this article explores effective alternatives to birth control for managing PCOS.
Understanding PCOS and Its Symptoms
PCOS is a complex endocrine disorder characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology. It is associated with disruptions in the hypothalamic-pituitary-ovarian (HPO) axis, leading to irregular menstrual cycles and anovulation. Elevated levels of luteinizing hormone (LH) relative to follicle-stimulating hormone (FSH) contribute to excessive ovarian androgen production, resulting in clinical manifestations such as hirsutism, acne, and alopecia.
Insulin resistance is a central feature of PCOS, affecting up to 70% of individuals with the condition. Hyperinsulinemia exacerbates ovarian androgen secretion and inhibits hepatic production of sex hormone-binding globulin (SHBG), further increasing circulating free androgens. This metabolic dysfunction predisposes individuals to weight gain, dyslipidemia, and an increased risk of type 2 diabetes and cardiovascular disease.
Additionally, PCOS is associated with chronic low-grade inflammation, as evidenced by elevated levels of inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6). These inflammatory pathways may contribute to the pathophysiology of insulin resistance and ovarian dysfunction. Given the heterogeneity of PCOS phenotypes, a personalized and multifaceted approach that addresses both endocrine and metabolic abnormalities is essential for effective symptom management.
1. Nutrition for PCOS Management
Diet plays a crucial role in managing PCOS symptoms. The right food choices can help regulate blood sugar levels, reduce inflammation, and balance hormones.
Prioritize Whole, Nutrient-Dense Foods
A diet rich in whole, unprocessed foods can significantly improve PCOS symptoms. Key dietary guidelines include:
- Low Glycemic Index (GI) Carbohydrates: Foods like whole grains, legumes, and non-starchy vegetables help regulate blood sugar levels.
- Healthy Fats: Incorporating sources such as avocados, nuts, seeds, and olive oil can improve insulin sensitivity and support hormone production.
- Lean Proteins: Chicken, fish, tofu, and legumes can help maintain stable blood sugar and support muscle mass.
Reduce Inflammatory Foods
Chronic inflammation is a common feature of PCOS. To minimize inflammation, avoid:
- Processed foods high in seed oils and refined sugars
- Excessive dairy and gluten (which may exacerbate inflammation in some individuals)
- Artificial additives and preservatives
Support Gut Health
The gut microbiome plays a significant role in hormone regulation. Probiotic-rich foods such as yogurt, kefir, kimchi, and sauerkraut can improve gut health and support metabolic balance.
2. Exercise and Movement
Regular physical activity is one of the most effective ways to improve insulin sensitivity, regulate menstrual cycles, and manage weight with PCOS.
Strength Training
Resistance training, including weight lifting and bodyweight exercises, can enhance insulin sensitivity, support lean muscle mass, and improve metabolic health.
Cardio Workouts
Moderate-intensity cardio exercises like brisk walking, cycling, or swimming can improve cardiovascular health and help with weight management.
Mindful Movement
Yoga and Pilates can help lower cortisol (stress hormone) levels and improve hormone balance, making them beneficial for managing PCOS symptoms.
3. Brown Fat and PCOS
Recent research has highlighted the potential role of brown adipose tissue (BAT), commonly known as brown fat, in managing Polycystic Ovary Syndrome (PCOS). Unlike white fat, which stores energy, brown fat burns calories to generate heat, thereby enhancing metabolism. This thermogenic property of brown fat can improve insulin sensitivity and metabolic health, which are often compromised in women with PCOS.
Strategies to Activate Brown Fat:
- Cold Exposure: Regular exposure to cold temperatures can stimulate brown fat activity. Practices such as cold showers or spending time in cooler environments may enhance BAT function.
- High-Intensity Interval Training (HIIT): Engaging in HIIT exercises has been associated with increased brown fat activation, contributing to improved metabolic outcomes.
- Dietary Choices: Consuming foods rich in healthy fats, particularly omega-3 fatty acids found in fish oil and flaxseeds, may support brown fat activity and overall metabolic health.
Incorporating these strategies into a holistic lifestyle approach may offer additional benefits for managing PCOS symptoms, complementing other interventions such as nutrition, exercise, stress management, and supplementation.
4. Stress Management and Sleep
Chronic stress and poor sleep can worsen PCOS symptoms by elevating cortisol levels and disrupting hormonal balance.
Stress-Reduction Techniques
- Meditation and Deep Breathing: Practicing mindfulness and controlled breathing can help reduce stress hormones.
- Journaling and Therapy: Expressing emotions and seeking professional support can help manage stress and anxiety related to PCOS.
- Spending Time in Nature: Outdoor activities and exposure to sunlight can help regulate circadian rhythms and improve mood.
Prioritizing Quality Sleep
- Maintain a Consistent Sleep Schedule: Going to bed and waking up at the same time each day supports hormonal balance.
- Limit Screen Time Before Bed: Blue light exposure from screens can disrupt melatonin production, affecting sleep quality.
- Create a Restful Sleep Environment: Keep your bedroom cool, dark, and free from distractions to promote deep sleep.
5. Natural Supplements for PCOS
Several supplements have been shown to support hormonal balance and improve PCOS symptoms.
Inositol
Myo-inositol and D-chiro-inositol are B-vitamin-like compounds that improve insulin sensitivity and ovarian function, helping to regulate menstrual cycles and reduce androgen levels.
Omega-3 Fatty Acids
Found in fish oil and flaxseeds, omega-3s help reduce inflammation, support heart health, and may improve insulin resistance in women with PCOS.
Vitamin D
Many women with PCOS have low vitamin D levels, which can contribute to insulin resistance and hormonal imbalances. Supplementing with vitamin D can improve metabolic and reproductive health.
Magnesium
Magnesium supports muscle relaxation, reduces inflammation, and helps regulate blood sugar levels, making it beneficial for women with PCOS.
6. NAC Over Metformin
N-Acetylcysteine (NAC) is gaining attention as a natural alternative to metformin for managing insulin resistance in PCOS.
NAC has been shown to:
- Improve insulin sensitivity
- Reduce oxidative stress and inflammation
- Support detoxification and liver health
- Promote ovulation and improve fertility outcomes
While metformin is a commonly prescribed medication for PCOS-related insulin resistance, it often comes with gastrointestinal side effects. NAC provides similar benefits without the discomfort, making it a promising option for those looking for natural interventions.
7. Alternative Therapies
Holistic approaches can complement lifestyle changes and provide additional support for PCOS management.
Acupuncture
Acupuncture has been found to improve ovulation, reduce androgen levels, and enhance insulin sensitivity in women with PCOS.
Herbal Medicine
- Spearmint Tea: Studies suggest that drinking spearmint tea may help lower testosterone levels and reduce hirsutism (excess hair growth).
- Cinnamon: This common spice has been shown to improve insulin sensitivity and regulate menstrual cycles in women with PCOS.
- Licorice Root: Used in traditional medicine, licorice root may help reduce androgen levels and support adrenal health.
8. Managing PCOS and Fertility
For women trying to conceive, lifestyle and dietary changes can significantly improve fertility outcomes without the need for birth control or medication.
Maintain a Healthy Weight
Even a modest weight loss of 5-10% can improve ovulation and increase the chances of conception.
Track Ovulation
Using basal body temperature (BBT) charting or ovulation predictor kits can help women with PCOS identify their most fertile days.
Consider Fertility-Supporting Supplements
Coenzyme Q10 (CoQ10), N-acetylcysteine (NAC), and vitamin B complex can support egg quality and reproductive function.
Conclusion
While birth control pills can be effective for managing PCOS symptoms, they are not the only solution. A holistic approach that includes dietary changes, exercise, stress management, and alternative therapies can provide long-term relief and improve overall well-being. Every woman’s journey with PCOS is unique, and finding the right combination of lifestyle modifications and natural treatments can empower individuals to take control of their health.

Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC9160465
https://doi.org/10.1002/ptr.2900
https://obgyn.onlinelibrary.wiley.com/doi/10.1111/j.1447-0756.2012.01844.x
https://ijmr.org.in/issue/2015-142-3
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-02817-2
https://www.degruyter.com/document/doi/10.7556/jaoa.2020.050/html
Ovulation is a fundamental aspect of reproductive health, marking the release of a mature egg from the ovary. This process is not only essential for conception but also serves as a key indicator of overall health, reflecting hormonal balance, metabolic stability, and adequate nutrient intake. However, various factors—including stress, sleep, and lifestyle choices—can influence ovulatory function. Among these, nutrition plays one of the most significant roles in regulating ovulation, supporting hormone production, and enhancing fertility.
Dietary choices directly affect ovarian function, with certain nutrients promoting hormonal equilibrium, follicular development, and cycle regularity, while others may contribute to anovulation, irregular cycles, and hormonal imbalances. Understanding the connection between nutrition and ovulation can empower individuals to make informed dietary choices that support reproductive health.

Understanding Ovulation and Its Importance
Ovulation occurs mid-cycle, typically around day 14 of a 28-day cycle, when a surge in luteinizing hormone (LH) triggers the release of a mature egg. This event is crucial for natural conception, as fertilization can only occur if a viable egg is available. However, ovulation is more than just a fertility marker—it is a reflection of a woman’s overall health.
Regular ovulation is associated with:
- Hormonal balance – The interplay of estrogen, progesterone, LH, and follicle-stimulating hormone (FSH) ensures normal menstrual cycles and reproductive health.
- Bone health – Estrogen, which fluctuates during the menstrual cycle, plays a key role in calcium absorption and maintaining bone density. Disruptions in ovulation can contribute to long-term skeletal issues such as osteoporosis.
- Cardiovascular function – Estrogen is also essential for heart health, helping regulate cholesterol levels and protect against cardiovascular disease. Women with irregular ovulation often have higher risks of heart disease due to hormonal imbalances.
- Metabolic stability – Regular ovulation is linked to better insulin sensitivity and stable blood sugar levels, reducing the risk of developing metabolic conditions such as type 2 diabetes.
On the other hand, disruptions in ovulation—such as anovulation (lack of ovulation), irregular cycles, or skipped periods—can signal underlying health concerns. Conditions like polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, thyroid dysfunction, and insulin resistance often present with ovulatory disturbances. These conditions can be influenced by diet, exercise, stress, and other lifestyle factors, making nutritional strategies an essential component of ovulatory health.
Key Nutrients That Support Ovulation
Several vitamins and minerals are essential for healthy ovulation and menstrual cycle regulation.
Folate (Vitamin B9)
Folate is critical for DNA synthesis, cell division, and hormone regulation. While it is widely recognized for its role in preventing neural tube defects, research shows that adequate folate intake can enhance ovulatory function. A 2023 study found that women with higher folate levels had a lower risk of ovulatory disorders and improved fertility outcomes.
Best sources: Leafy greens (spinach, kale), lentils, chickpeas, asparagus, and avocados.

Inositol (Myo-Inositol & D-Chiro-Inositol)
Inositol, particularly myo-inositol, plays a crucial role in insulin signaling and ovarian function. Insulin resistance is a major contributor to ovulatory dysfunction, particularly in women with PCOS. Studies suggest that inositol supplementation can improve insulin sensitivity, regulate menstrual cycles, and enhance ovulation rates.
- Best sources: Citrus fruits, whole grains, beans, and nuts.
Omega-3 Fatty Acids
Omega-3s reduce inflammation, support hormone synthesis, and regulate menstrual cycles. Research published in Prostaglandins, Leukotrienes & Essential Fatty Acids found that omega-3 supplementation is associated with improved ovulatory function and reduced risk of anovulation.
- Best sources: Fatty fish (salmon, sardines, mackerel), flaxseeds, walnuts, chia seeds.
Vitamin D
Vitamin D plays a role in modulating reproductive hormones, including FSH and anti-Müllerian hormone (AMH), which are essential for ovarian reserve and egg quality. Deficiency has been linked to irregular cycles and ovulatory dysfunction.
- Best sources: Sun exposure, fortified dairy products, egg yolks, and fatty fish.
Zinc
Zinc is essential for follicular development, egg maturation, and progesterone production. A deficiency can lead to delayed ovulation and reduced fertility.
Best sources: Oysters, pumpkin seeds, chickpeas, beef, and cashews.

Magnesium
Magnesium is crucial for hormonal balance, stress regulation, and progesterone production. Research suggests that magnesium supplementation can support ovulatory function and improve menstrual cycle regularity.
- Best sources: Leafy greens, almonds, dark chocolate, and bananas.
Dietary Patterns for Optimal Ovulation
Beyond individual nutrients, overall dietary patterns significantly influence ovulation and fertility.
The Mediterranean Diet

A Mediterranean-style diet, rich in anti-inflammatory and nutrient-dense foods, is associated with higher fertility rates and improved ovulatory function.
Key components:
✔ Fatty fish (rich in omega-3s)
✔ Fresh fruits and vegetables (high in antioxidants)
✔ Whole grains and legumes (low glycemic index)
✔ Healthy fats (olive oil, nuts, seeds)
Low Glycemic Index (GI) Diet
A low-GI diet stabilizes blood sugar levels and improves insulin sensitivity, which is particularly beneficial for women with PCOS-related ovulatory dysfunction.
Anti-Inflammatory Diet
Chronic inflammation contributes to hormonal imbalances and ovulatory irregularities. An anti-inflammatory diet includes omega-3-rich foods, leafy greens, nuts, and herbs like turmeric and ginger.
Foods and Habits That Can Disrupt Ovulation
Certain dietary and lifestyle factors can negatively impact reproductive health:
Excess sugar and refined carbs – Can increase insulin resistance, disrupting ovulation.
Trans fats and processed foods – Linked to increased inflammation and hormonal imbalances.
Excess caffeine and alcohol – Can interfere with reproductive hormones and lower fertility.
Extreme dieting or under-eating – Can cause hypothalamic amenorrhea, leading to ovulation loss.
Lifestyle Factors That Enhance Ovulation
Beyond diet, several lifestyle factors can improve ovulatory function:
✔ Regular Exercise – Moderate activity supports hormone regulation, while excessive high-intensity exercise may negatively impact ovulation.
✔ Stress Management – Chronic stress elevates cortisol, which can suppress ovulation. Mindfulness, yoga, and meditation help reduce stress-related hormonal disruptions.
✔ Quality Sleep – Poor sleep disrupts reproductive hormones, leading to irregular cycles and ovulatory dysfunction. Aim for 7-9 hours of quality sleep per night.
Quality Prenatals and the MTHFR Gene
When preparing for pregnancy or supporting reproductive health, taking a high-quality prenatal vitamin is essential. Prenatals help ensure that women get the key nutrients needed for healthy ovulation and a successful pregnancy, even before conception occurs. A quality prenatal should contain at least 400-800 mcg of methylated folate, iron, calcium, vitamin D, iodine, and omega-3 fatty acids.

When to Start Taking Prenatals:
It’s advisable to begin taking prenatal vitamins at least 1-3 months before trying to conceive. This allows the body to build up stores of essential nutrients, particularly folate, which is crucial for fetal development and preventing neural tube defects. If there’s a known issue with ovulation or other reproductive health concerns, starting prenatal vitamins earlier can be beneficial.
Choosing a Quality Prenatal: Not all prenatal vitamins are created equal. Look for brands that are third-party tested for purity and potency. Some reputable brands include:
- FullWell – Known for its high-quality, bioavailable ingredients, including methylated folate for optimal absorption.
- Seeking Health – Offers a comprehensive prenatal formula with L-methylfolate and other key nutrients for reproductive health.
- Needed – A newer brand with an emphasis on clean, evidence-based ingredients, including methylated folate and Omega-3s.
- Thorne Research – Offers a highly bioavailable form of folate (L-methylfolate) and is known for its rigorous testing standards.
- Theralogix – Provides a well-rounded prenatal with the active form of folate (5-MTHF), ensuring better absorption and supporting overall fertility.
MTHFR Gene and Methylated Folate: The MTHFR gene plays a critical role in processing folate in the body. People with certain mutations in the MTHFR gene may have difficulty converting synthetic folic acid into its active form, 5-methyltetrahydrofolate (methylated folate). This can lead to higher homocysteine levels, which may increase the risk of cardiovascular issues and reproductive complications, including difficulty with conception.
For those with an MTHFR mutation, taking methylated folate instead of regular folic acid is recommended. Methylated folate is the form the body can directly use, making it more effective for those with MTHFR gene mutations. Many high-quality prenatal vitamins offer methylated folate (often labeled as L-methylfolate or 5-MTHF) to bypass the need for the conversion process.
Before starting a prenatal vitamin regimen, especially if there’s a concern about MTHFR mutations or other health issues, it’s always wise to consult with a healthcare provider or registered dietitian to ensure you’re selecting the best prenatal and dosage for your needs.
Final Thoughts
Ovulation is not just about fertility—it is a vital indicator of overall health. A nutrient-rich, anti-inflammatory diet and a balanced lifestyle can enhance ovulatory function, regulate menstrual cycles, and support fertility potential. If you experience irregular ovulation, consider working with a registered dietitian or healthcare provider to develop a personalized nutrition and lifestyle plan tailored to your needs.
By making small but meaningful dietary and lifestyle adjustments, you can optimize ovulation and support long-term reproductive health.
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC11215161
https://pmc.ncbi.nlm.nih.gov/articles/PMC10475284/#s0005
https://www.sciencedirect.com/science/article/pii/S1389945706006216
https://pmc.ncbi.nlm.nih.gov/articles/PMC11013220
https://pmc.ncbi.nlm.nih.gov/articles/PMC8634384/#:~:text=Conversely%2C%20a%20diet%20based%20on,positive%20impact%20on%20female%20fertility https://pmc.ncbi.nlm.nih.gov/articles/PMC10309424/

Secondary infertility—the challenge of conceiving or carrying a pregnancy to term after previously giving birth—can be an emotional and frustrating experience for many families. But just remember: you’re not alone. This condition affects about 10% of couples. The good news is that functional nutrition offers an empowering way to address some of the root causes of secondary infertility, supporting your body and boosting your chances of growing your family. In this post, we’ll explore evidence-based nutritional strategies to help you on your journey.

Secondary infertility is complex, with causes ranging from hormonal imbalances and structural issues to lifestyle factors like stress and diet. Age-related fertility changes, ovulation disorders, diminished ovarian reserve, and male infertility are common culprits. Functional nutrition focuses on addressing these root causes through personalized dietary and lifestyle changes, helping to create the best possible conditions for conception and a healthy pregnancy.
How Functional Nutrition Supports Fertility
Functional nutrition takes a whole-person approach, targeting underlying factors that might be affecting your fertility. From reducing inflammation to balancing hormones, these strategies are here to support your health and your baby dreams. Let’s dive into the key areas:
1. Taming Oxidative Stress
Oxidative stress—an imbalance between damaging free radicals and protective antioxidants—can harm both egg and sperm quality. Research reveals that oxidative stress disrupts hormone production and even affects embryo implantation.
Oxidative stress is particularly problematic because it can reduce ovarian reserve and negatively impact sperm motility and morphology. Studies emphasize the importance of addressing oxidative damage to improve reproductive outcomes. Furthermore, chronic oxidative stress can exacerbate conditions like endometriosis and polycystic ovary syndrome (PCOS), compounding fertility challenges.

Here’s how to tackle oxidative stress:
- Eat Your Antioxidants: Fill your plate with colorful fruits and veggies like berries, oranges, spinach, and bell peppers. Antioxidant-rich foods combat oxidative damage and protect reproductive cells.
- Boost Omega-3s: Fatty fish like salmon and plant-based options like flaxseeds and walnuts help lower inflammation and protect against oxidative stress.
- Consider CoQ10: This powerful antioxidant, found in organ meats and supplements, improves mitochondrial function in eggs and sperm, enhancing their quality and viability.
- Include Vitamin E and C: These vitamins work synergistically to neutralize free radicals and improve reproductive outcomes. Nuts, seeds, citrus fruits, and strawberries are excellent sources.
- Explore Selenium and Glutathione: Selenium, found in Brazil nuts, and glutathione, synthesized within the body, are essential antioxidants that play key roles in reducing oxidative stress in reproductive tissues
2. Balancing Hormones Naturally
Hormonal imbalances are a common barrier to conception. Functional nutrition can help stabilize blood sugar, enhance liver detoxification, and supply key nutrients to support hormone health:
- Balance Blood Sugar: Swap refined carbs for whole grains, legumes, and veggies to avoid insulin spikes, which can throw hormones out of sync. Studies have shown that stable blood sugar levels support ovulation and reduce symptoms of PCOS.
- Support Your Liver: Include cruciferous veggies like broccoli, kale, and Brussels sprouts to help your body metabolize hormones effectively. Your liver plays a crucial role in detoxifying excess estrogen, maintaining hormonal harmony.
- Power Up with Micronutrients: Zinc (in pumpkin seeds and oysters), magnesium (in spinach and almonds), and vitamin B6 (in bananas and chickpeas) are all hormone heroes. Research highlights the importance of these nutrients in regulating the menstrual cycle and promoting fertility.
- Manage Stress Hormones: Chronic stress can disrupt the delicate balance of reproductive hormones. Incorporate stress-relief practices like yoga, meditation, or even gentle walks in nature alongside stress-adaptable foods like leafy greens and whole grains.
- Include Healthy Fats: Omega-3 fatty acids found in fish, walnuts, and chia seeds help build the building blocks of reproductive hormones while reducing inflammation.
3. Prioritizing Gut Health
Your gut health impacts everything from inflammation to hormone regulation. An imbalance in gut bacteria, called dysbiosis, can disrupt reproductive health. Emerging research shows the connection between gut microbiota and fertility, with gut health influencing hormone metabolism, immune function, and nutrient absorption
Studies show that:
- Gut Dysbiosis Affects Hormonal Balance: An imbalanced microbiome can interfere with estrogen metabolism, potentially leading to conditions like PCOS and endometriosis that hinder fertility.
- A Healthy Gut Reduces Inflammation: A diverse and balanced microbiome helps lower systemic inflammation, creating a more favorable environment for conception.
- Probiotic Support Can Boost Fertility: Specific probiotic strains have been shown to improve reproductive health by modulating the immune system and supporting a balanced microbiota.
Here’s how to nurture your gut:
- Load Up on Fiber: Whole grains, fruits, and veggies provide prebiotic fiber that feeds beneficial gut bacteria. Fiber-rich foods also help eliminate excess hormones, maintaining hormonal balance.
- Try Fermented Foods: Yogurt, kefir, kimchi, and sauerkraut are rich in probiotics that support a healthy gut microbiome.
- Add Probiotic Supplements: Consider strains like Lactobacillus and Bifidobacterium, which have been shown to improve gut and reproductive health. Always consult with a healthcare provider before starting any supplement regimen.
- Skip Processed Foods: Refined sugars and additives can harm your gut microbiome and increase inflammation. Focus on whole, nutrient-dense foods to support gut health and fertility.
- Hydrate Well: Drinking plenty of water aids digestion and supports the gut lining, promoting overall gut health.

4. Filling Nutrient Gaps
Certain nutrient deficiencies can hinder fertility. Functional nutrition ensures you’re getting enough of the essentials:
- Folate: Found in leafy greens, lentils, and fortified cereals, folate supports egg quality and early fetal development. Studies show folate also plays a critical role in reducing neural tube defects and supporting sperm health.
- Vitamin D: This sunshine vitamin is linked to better fertility and pregnancy outcomes. Enjoy fatty fish, fortified milk, or a walk in the sun to keep levels up. Research highlights its role in improving ovarian function and endometrial health.
- Iron: Essential for ovulation and pregnancy, iron is abundant in lean meats, beans, and dark leafy greens. Low iron levels can disrupt ovulatory cycles and impact embryo implantation.
- Vitamin B12: Found in eggs, dairy, and fortified foods, this nutrient supports red blood cell production and neurological health, both of which are critical for a healthy pregnancy.
- Choline: Often overlooked, choline, found in eggs and fish, is vital for fetal brain development and placental function.
5. Stress Less for Better Fertility
Stress has a profound impact on fertility by disrupting the hormonal balance necessary for ovulation and implantation. Chronic stress triggers the release of cortisol and other stress hormones, which can suppress the production of reproductive hormones like luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This hormonal imbalance may lead to irregular menstrual cycles and impaired ovulation, making conception more challenging.
Evidence-Backed Strategies to Reduce Stress:
- Mind-Body Interventions: Practices like yoga, meditation, and mindfulness-based stress reduction (MBSR) have been shown to decrease cortisol levels and improve fertility outcomes. MBSR can enhance emotional resilience, which is crucial for couples navigating the challenges of secondary infertility.
- Regular Physical Activity: Moderate-intensity exercise like walking, swimming, or cycling helps lower stress hormone levels and improve mood. However, it’s essential to avoid overtraining, as excessive physical stress can negatively impact ovulation.
- Cognitive Behavioral Therapy (CBT): CBT has been effective in reducing stress-related infertility. It helps individuals reframe negative thoughts and develop coping mechanisms, ultimately improving reproductive outcomes.
- Dietary Support: Foods rich in magnesium (dark leafy greens, nuts, seeds) and adaptogenic herbs like ashwagandha may help regulate the hypothalamic-pituitary-adrenal (HPA) axis, reducing cortisol levels and improving hormonal harmony.
- Social Support and Counseling: Emotional support from partners, friends, or support groups can significantly reduce stress and improve mental health during the journey of secondary infertility.

6. Don’t Forget Male Fertility
Male fertility plays an equally critical role in conception, with sperm quality being a significant factor in secondary infertility. Up to 50% of infertility cases involve male factors, such as low sperm count, poor motility, or abnormal morphology.
- Antioxidant Supplementation: Oxidative stress is a major contributor to sperm dysfunction. Antioxidants like CoQ10, vitamin C, and selenium have been shown to improve sperm motility, count, and overall quality (PubMed 33750412, PMC6102891). A daily intake of CoQ10, for instance, enhances mitochondrial function in sperm, leading to improved motility and fertilization capacity.
- Lifestyle Adjustments: Reducing alcohol and tobacco use is essential, as both have been linked to sperm DNA damage and reduced motility (PubMed 15327187). Limiting exposure to environmental toxins, such as pesticides and heavy metals, can further protect sperm health (PMC10956697).
Nutritional Support:
- Zinc and Selenium: Found in oysters, Brazil nuts, and seeds, these trace minerals are critical for sperm production and protection against oxidative stress.
- Folate and B12: These vitamins support DNA synthesis and repair in sperm, reducing the risk of chromosomal abnormalities.
Healthy Weight Management: Obesity negatively affects testosterone levels and sperm quality. Adopting a balanced diet and regular exercise routine can improve hormonal balance and reproductive outcomes.
Regular Medical Check-Ups: Conditions like varicocele, hormonal imbalances, or infections can impair sperm quality. Early diagnosis and treatment of underlying issues significantly enhance fertility potential.
Your Action Plan for Functional Nutrition
Ready to take charge? Here are some steps to get started:
- Identify and Address Deficiencies: Partner with a healthcare provider to test for and correct nutrient gaps.
- Adopt a Whole-Foods Approach: Stick to nutrient-dense, minimally processed foods for maximum health benefits.
- Avoid Toxins: Limit exposure to endocrine-disrupting chemicals in plastics, pesticides, and cosmetics.
- Track Your Cycle: Monitoring your menstrual cycle can reveal patterns and help time conception.
- Prioritize Rest and Movement: Moderate exercise and quality sleep are vital for hormonal balance and stress management.
The Bottom Line
Secondary infertility can be a challenging journey, but it’s one you don’t have to face alone. Functional nutrition offers a hopeful path forward by addressing the root causes of infertility and optimizing your body for conception. By nourishing yourself with the right foods, reducing stress, and supporting your overall health, you’re giving your body the best chance to thrive.
If you’re struggling with secondary infertility, consider reaching out to a functional nutrition expert for a personalized plan. With the right tools and support, your family dreams are within reach. Here’s to hope, health, and new beginnings!
Sources
https://my.clevelandclinic.org/health/diseases/21139-secondary-infertility
https://pubmed.ncbi.nlm.nih.gov/15327187
https://pubmed.ncbi.nlm.nih.gov/28677273
https://pubmed.ncbi.nlm.nih.gov/33750412
https://pmc.ncbi.nlm.nih.gov/articles/PMC10956697
https://pmc.ncbi.nlm.nih.gov/articles/PMC10766669
https://pmc.ncbi.nlm.nih.gov/articles/PMC10608597
https://rep.bioscientifica.com/view/journals/rep/164/6/REP-22-0152.xml
https://pmc.ncbi.nlm.nih.gov/articles/PMC6102891
https://pmc.ncbi.nlm.nih.gov/articles/PMC9800796
https://pmc.ncbi.nlm.nih.gov/articles/PMC8582214
https://pubmed.ncbi.nlm.nih.gov/34918486/ https://pmc.ncbi.nlm.nih.gov/articles/PMC10349861/
The postpartum period is a transformative and challenging time for new mothers. As you care for your newborn, your own health often takes a backseat. However, prioritizing nutrition is essential for recovery, energy, and overall well-being. Here, we’ll explore the key nutritional considerations for postpartum moms, supported by expert insights and practical tips.

1. Supporting Hormonal Balance
After childbirth, your hormone levels experience significant fluctuations. Estrogen and progesterone drop rapidly, while prolactin rises to support breastfeeding. This hormonal upheaval can contribute to mood swings, fatigue, and even postpartum depression.
Key Nutrients to Focus On:
- Healthy Fats: Omega-3 fatty acids, particularly DHA and EPA, found in salmon, sardines, walnuts, and flaxseeds, support brain health and may help stabilize mood. Research highlights that omega-3s can also play a role in reducing inflammation and supporting cognitive function during the postpartum period. Additionally, these fats are essential for the development of the baby’s brain and nervous system, especially during breastfeeding.
- B Vitamins: These are crucial for neurotransmitter production, which helps combat “mommy brain” and postpartum depression. Vitamin B6, found in salmon, poultry, and bananas, aids serotonin production, while B12, abundant in eggs and lean meats, supports energy metabolism and neurological health. Studies link B vitamin deficiencies to mood disorders, emphasizing their importance during postpartum recovery.
- Magnesium: This essential mineral helps regulate stress, improve sleep quality, and support muscle recovery. Found in dark leafy greens, nuts, seeds, and whole grains, magnesium’s calming effects are particularly beneficial for new moms facing sleep deprivation and stress.
Lifestyle Tip: Adaptogenic herbs like ashwagandha and Rhodiola can help balance cortisol levels and support adrenal health, which are often compromised during the postpartum period. These herbs may aid in reducing fatigue and enhancing resilience to stress, but they should be used under professional guidance
2. Boosting Energy Levels
Fatigue is a common postpartum challenge, often exacerbated by interrupted sleep and physical recovery from childbirth. Nutritional strategies can play a pivotal role in boosting your energy reserves.

Key Foods for Sustained Energy:
- Complex Carbohydrates: Foods like sweet potatoes, quinoa, and oats are rich in fiber and slow-digesting carbohydrates that provide steady energy throughout the day. These complex carbs help prevent energy crashes by stabilizing blood sugar levels.
- Protein-Rich Foods: Protein is essential for muscle repair, recovery, and sustained energy. Incorporate eggs, lean meats, tofu, and legumes into your meals. Protein also supports satiety, helping you stay energized and focused for longer periods of time.
- Iron-Rich Foods: Postpartum moms are at an increased risk of iron deficiency, especially after blood loss during delivery. Include iron-rich foods like spinach, red meat, and lentils in your diet. Pair these with vitamin C-rich foods (bell peppers, citrus fruits) to enhance absorption and combat fatigue associated with anemia
- Healthy Fats: Don’t overlook the importance of healthy fats like avocados, olive oil, and nuts, which provide a slow-burning source of energy and support overall cellular health.
Hydration: Dehydration can exacerbate feelings of fatigue and hinder milk production for breastfeeding mothers. Aim for at least 8-10 glasses of water daily, and consider incorporating herbal teas or electrolyte-rich drinks for added hydration. Keep a water bottle handy to remind yourself to sip throughout the day.Snack Smart: Opt for nutrient-dense snacks that combine protein, healthy fats, and complex carbs to maintain steady energy levels. Examples include Greek yogurt with granola, apple slices with almond butter, or hummus with whole-grain crackers.
3. Enhancing Breastfeeding Nutrition

For breastfeeding moms, the nutritional demands increase significantly. Breast milk production requires an additional 450-500 calories per day, along with a higher intake of certain nutrients.
Breastfeeding-Friendly Nutrients:
- Calcium and Vitamin D: Essential for maintaining bone health, these nutrients are crucial for both mom and baby. Calcium can be found in dairy products, fortified plant-based milks, almonds, and dark leafy greens, while vitamin D can be obtained from fortified foods and sunlight exposure. Adequate vitamin D is particularly vital for preventing bone demineralization in breastfeeding moms.
- Zinc: This mineral is critical for immune function and cellular repair. Zinc is abundant in foods like shellfish, legumes, nuts, seeds, and whole grains. Its role in wound healing is especially important for moms recovering from childbirth or C-sections.
- Choline: Found in eggs, liver, and fish, choline is vital for infant brain development and maternal cognitive function. Research emphasizes the importance of choline for neurodevelopment, particularly during lactation.
Foods to Avoid or Limit:
- Caffeine: While small amounts are generally safe, excessive caffeine can pass into breast milk and disrupt your baby’s sleep patterns. Limit intake to one to two cups of coffee per day.
- Alcohol: Alcohol can also pass into breast milk and affect your baby’s development. If you choose to drink, wait at least two hours per drink before breastfeeding to allow your body to metabolize the alcohol.
Snack Ideas for Breastfeeding Moms:
- Greek yogurt with berries and granola: Provides calcium, probiotics, and antioxidants.
- Hummus with carrot and cucumber sticks: Packed with fiber and plant-based protein.
Almond butter on whole-grain toast: A nutrient-dense snack rich in healthy fats, protein, and complex carbs.
4. Promoting Postpartum Recovery
Healing after childbirth requires specific nutrients to support tissue repair and combat inflammation. This is particularly important for moms recovering from C-sections or Healing after childbirth requires specific nutrients to support tissue repair and combat inflammation. This is particularly important for moms recovering from C-sections or perineal tears.

Recovery-Boosting Foods:
- Collagen-Rich Foods: Foods like bone broth, chicken skin, and gelatin provide collagen, a structural protein that aids in tissue repair and skin elasticity. Collagen is especially beneficial for healing wounds and repairing connective tissues stressed during childbirth.
- Vitamin C: This powerful antioxidant is vital for collagen production and wound healing. Include vitamin C-rich foods such as oranges, strawberries, bell peppers, and broccoli in your diet to support tissue regeneration and enhance your immune system.
- Anti-Inflammatory Foods: Turmeric, ginger, and fatty fish like salmon and mackerel are rich in anti-inflammatory compounds. These foods help reduce inflammation, promote faster recovery, and alleviate postpartum discomfort.
5. Addressing Postpartum Hair Loss
Many moms experience postpartum hair loss due to hormonal changes. While this is usually temporary, certain nutrients can support hair regrowth.
Key Nutrients for Hair Health:
- Biotin: Found in eggs, nuts, seeds, and sweet potatoes, biotin strengthens hair and nails by supporting keratin production. Studies suggest that biotin supplementation can help reduce hair shedding and improve hair thickness.
- Iron and Zinc: Both minerals are crucial for healthy hair follicles and preventing excessive shedding. Iron-rich foods include lean meats, spinach, and lentils, while zinc can be obtained from shellfish, legumes, and some seeds like pumpkin, hemp, and chia. Iron deficiency anemia is a common postpartum issue that can exacerbate hair loss.
- Protein: Since hair is made of keratin, a structural protein, consuming adequate protein is essential for hair health. Incorporate lean meats, fish, eggs, and plant-based proteins like quinoa and tofu into your diet.
Lifestyle Tip: Avoid tight hairstyles and harsh treatments, such as excessive heat styling or chemical processes, which can weaken fragile postpartum hair. Opt for gentle, sulfate-free shampoos and conditioners enriched with nourishing ingredients like argan oil or keratin.
6. Preventing Postpartum Depression
Nutrition plays a significant role in mental health, and deficiencies in key nutrients can contribute to postpartum depression.

Mood-Boosting Nutrients:
- Omega-3 Fatty Acids: These essential fats, found in fatty fish like salmon, sardines, and algae-based supplements, are crucial for brain function and mood regulation. Research shows that omega-3s can help reduce the risk of postpartum depression (PPD) by supporting the brain’s ability to produce mood-regulating neurotransmitters like serotonin. For those who don’t consume fish, algae-based supplements offer a plant-based option that can help meet your omega-3 needs.
- Vitamin D: A deficiency in vitamin D has been strongly linked to depression. Adequate levels of vitamin D help regulate mood and may reduce the risk of PPD. Vitamin D is produced in the skin through sunlight exposure, but it can also be obtained through fortified foods and supplements.
- Probiotics: Gut health and mental health are deeply interconnected, with studies showing that a balanced gut microbiome can positively impact mood and reduce stress. Fermented foods like yogurt, kefir, kimchi, and sauerkraut, rich in beneficial bacteria, can support gut health and, in turn, emotional well-being.
Mindfulness Tip: Combine good nutrition with self-care practices like meditation, gentle exercise, and connecting with loved ones. These practices can help to reduce stress, support emotional resilience, and promote overall well-being during the postpartum period.
7. Practical Tips for Postpartum Nutrition
Balancing your own nutrition with the demands of a newborn can be overwhelming. Here are some practical strategies to make it easier:

Meal Prepping: Prepare and freeze nutrient-dense meals before delivery. This ensures you have access to nourishing food during the busy postpartum weeks. Consider meals with healthy fats, protein, and complex carbs to sustain your energy.
Nutrient-Dense Snacks: Keep easy, nutrient-packed snacks like trail mix, hard-boiled eggs, protein bars, and even pre-portioned fruit or veggie packs. These can help keep your blood sugar stable and give you the energy needed for breastfeeding and taking care of your baby.
Accept Help: Allow friends and family to assist with meal preparation, groceries, or even just getting a little extra sleep. It’s important to remember that self-care involves accepting support when needed.
Supplements: Consider a high-quality postpartum multivitamin and specific supplements like omega-3s and probiotics. These can help fill any nutritional gaps, especially if you’re feeling depleted during the early stages of motherhood. Always consult with your healthcare provider before starting any new supplements.
8. Long-Term Nutrition for Postpartum Health
The postpartum period extends beyond the initial weeks after birth. Continued attention to your diet can support long-term health and energy levels.

Key Focus Areas:
- Balance of Macronutrients:Maintaining a balance of carbohydrates, proteins, and fats is key for sustained energy. Whole foods, such as lean meats, legumes, and whole grains, provide necessary nutrients and help balance blood sugar, which is essential for both mood stability and physical recovery.
- Prioritize Whole, Unprocessed Foods: A diet rich in whole, unprocessed foods is beneficial for reducing inflammation, supporting hormonal balance, and providing the necessary nutrients for recovery. This includes incorporating fresh fruits and vegetables, healthy fats (like those from avocado, nuts, and olive oil), and quality protein sources (such as eggs, lean meat, and legumes). Anti-inflammatory foods like berries, leafy greens, and turmeric can also help reduce any postpartum swelling and improve recovery time.
- Stay Active: Gentle exercises, such as walking, yoga, or pilates, can be beneficial for postpartum recovery. These activities can help improve mood, reduce stress, and support physical recovery. Hormonal fluctuations can also contribute to fatigue and emotional highs and lows, but light movement can help regulate these changes over time. Avoid overexertion, especially if you’re still adjusting to your new physical condition.
- Adrenal Fatigue and Postpartum Care: Postpartum mothers often experience adrenal fatigue, which can exacerbate feelings of exhaustion and mood instability. This occurs due to the stress of labor, childbirth, and the transition to motherhood. To support your adrenal health, make sure you’re getting enough sleep, managing stress, and eating nutrient-dense foods rich in vitamin C (such as citrus fruits, bell peppers, and leafy greens) and B vitamins (found in whole grains and lean meats).
Conclusion
Postpartum nutrition is about more than just eating; it’s about nourishing your body, mind, and spirit as you navigate motherhood. By focusing on nutrient-dense foods, staying hydrated, and listening to your body’s needs, you can promote recovery, boost energy, and enhance overall well-being. Remember, taking care of yourself is not selfish—it’s essential for being the best mom you can be.
Your journey to postpartum health is unique, so tailor these recommendations to your personal needs and consult a healthcare professional for personalized guidance.
Sources:
https://drbrighten.com/adrenal-fatigue-mom
https://drbrighten.com/balance-hormones-while-breastfeeding
https://drbrighten.com/5-ways-to-improve-your-early-postpartum-care
https://drbrighten.com/8-ways-to-eliminate-postpartum-depression-and-be-free-of-mommy-brain
https://drbrighten.com/can-you-prevent-postpartum-hair-loss
https://pmc.ncbi.nlm.nih.gov/articles/PMC6380979
https://pubmed.ncbi.nlm.nih.gov/25573272
https://pubmed.ncbi.nlm.nih.gov/32357982/ https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0235806

Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Endometriosis—what a mouthful, right? This chronic condition affects an estimated 10% of women of reproductive age worldwide. But despite how common it is, endometriosis often feels like a lonely battle. Essentially, it involves endometrial-like tissue growing outside the uterus, leading to pain, infertility, and a host of other pesky symptoms. While traditional treatments like hormonal therapy and surgery can help, functional nutrition offers a fresh, empowering perspective.
Let’s dig into how the right foods can help you take charge of your health and tackle endometriosis head-on.
Let’s Break It Down: What Causes Endometriosis?
Spoiler alert: scientists are still piecing together the puzzle of endometriosis. While the exact cause remains unclear, research points to several contributing factors:
- Inflammation: Chronic inflammation plays a central role, fueling lesion growth and pain.
- Hormonal Imbalances: Estrogen dominance often exacerbates symptoms.
- Immune Dysregulation: The immune system may fail to recognize and clear out misplaced endometrial-like tissue.
- Oxidative Stress: Elevated oxidative stress can worsen symptoms by damaging tissues and promoting inflammation.
- Environmental Factors: Exposure to endocrine-disrupting chemicals (EDCs) like BPA and phthalates may increase your risk.
Good news? Many of these factors can be influenced by your diet and lifestyle choices. Let’s unpack the connection between what’s on your plate and how your body feels.
Inflammation and Food: The Connection
Inflammation is like the annoying party guest that just won’t leave—especially for those dealing with endometriosis. Here’s how your food choices can either fan the flames or help cool things down:
The Culprits
- Processed Foods: Packaged snacks, fast food, and sugary treats are loaded with additives that promote inflammation.
- Refined Carbohydrates: White bread, pasta, and other refined carbs cause blood sugar spikes, triggering inflammatory pathways.
- Seed Oils: Vegetable oils like soybean, corn, and sunflower oils are loaded with omega-6 fatty acids, which can exacerbate inflammation if not balanced by omega-3s or when consumed in excess.
The Heroes
- Fruits and Vegetables: Packed with antioxidants and phytochemicals, these help neutralize free radicals and reduce inflammation. Focus on leafy greens, berries, and cruciferous veggies like broccoli and cauliflower.
- Omega-3 Fatty Acids: Found in salmon, chia seeds, and walnuts, omega-3s reduce prostaglandins, compounds that worsen pain and inflammation.
- Herbs and Spices: Turmeric, ginger, and cinnamon have anti-inflammatory properties that can calm flare-ups.
Pro Tip
Adopting an anti-inflammatory diet doesn’t mean a complete overhaul overnight. Start small—swap out your usual snack for a handful of nuts, or add a side of roasted veggies to your dinner. Every bite counts!
Eat This, Not That: Functional Nutrition for Endometriosis
Functional nutrition isn’t about deprivation—it’s about giving your body the tools it needs to thrive. Let’s dive into some strategies:
1. Fight Fire with Food: Anti-Inflammatory Diet
Inflammation is the not-so-secret villain in the endometriosis saga. Luckily, you can put out the flames with foods rich in omega-3s, like salmon, walnuts, and flaxseeds. These goodies help reduce prostaglandin production, which means less pain.
Load up on: Leafy greens, berries, turmeric, and ginger—nature’s anti-inflammatory superstars.
Steer clear of: Processed foods, seed oils and sugary treats. Sorry, donut lovers.
2. Hormonal Harmony: Balancing Estrogen
Estrogen dominance is a common villain in the endometriosis story. When estrogen levels are out of whack, it can exacerbate symptoms like pain and bloating. Here’s how to bring balance back:
- Cruciferous Vegetables: Broccoli, kale, and Brussels sprouts contain indole-3-carbinol, a compound that supports estrogen detoxification in the liver.
- Fiber-Rich Foods: Whole grains, legumes, and flaxseeds help your gut efficiently excrete excess estrogen. Bonus: They also feed your friendly gut bacteria!
- Limit Alcohol and Caffeine: These can interfere with your liver’s ability to metabolize hormones, so moderation is key.
3. Gut Check: Heal from the Inside Out
Did you know your gut is like the command center for inflammation and hormones? A happy gut equals a healthier you. Here’s how to give it some love:
- Fermented Foods: Kimchi, sauerkraut, and yogurt are packed with probiotics that support a healthy microbiome.
- Prebiotics: Garlic, onions, and asparagus provide food for your gut’s good bacteria.
- Reduce Gut Irritants: Cut back on processed foods, artificial sweeteners, and excessive dairy if they’re causing distress.
A well-nourished gut can reduce systemic inflammation, support hormone balance, and even improve your mood—talk about multitasking!
4. Oxidative Stress, Be Gone
Endometriosis often goes hand-in-hand with oxidative stress. Antioxidants to the rescue! Vitamin C from oranges and polyphenols from green tea are your secret weapons against free radicals. Studies show that antioxidants may help reduce the oxidative stress associated with endometriosis, alleviating pain and inflammation.
5. Magnesium and Zinc: The Dynamic Duo
Crampy? Magnesium-rich foods like spinach and dark chocolate (yay!) can help. Magnesium plays a key role in muscle relaxation and can soothe the cramps that are so common with endometriosis. Zinc, found in pumpkin seeds and lean meats, supports your immune system and calms inflammation, making it an excellent mineral for those dealing with this condition.
Supplements: Small Pills, Big Impact
Supplements can complement your diet and fill in gaps that food alone may not cover. While not a cure-all, they can be powerful allies when used correctly. Here’s the lowdown:
• Omega-3 Fatty Acids: These healthy fats are like the bodyguards of your body, especially when it comes to inflammation. Omega-3s, found in fish oil or algae-based supplements, are potent inflammation fighters. They work by reducing the production of prostaglandins—those pesky compounds that increase pain and inflammation in the body. Consuming omega-3s regularly has been linked to a reduction in endometriosis-related pain, making them an essential part of any functional nutrition plan.
• Vitamin D: Vitamin D isn’t just for strong bones; it also plays a critical role in immune function and hormone regulation. Studies have found that low levels of vitamin D are often associated with more severe symptoms of endometriosis. This sunshine vitamin can help regulate your immune system and may even shrink those troublesome lesions over time. Just a heads up—vitamin D is fat-soluble, so it’s best absorbed when taken with a fat-containing meal, like avocado or olive oil.
• Curcumin: Derived from the golden root of turmeric, curcumin is a superstar in the world of anti-inflammatory supplements. It’s known for its ability to reduce inflammation and alleviate pain, which is especially important for managing endometriosis flare-ups. But wait—there’s more! Studies suggest that curcumin can also inhibit the growth of endometrial tissue, potentially slowing the progression of the condition. Plus, curcumin is a multitasker; it supports joint and gut health, making it an all-around wellness booster.
• N-Acetyl Cysteine (NAC): This powerful antioxidant is a detox champion. NAC helps to reduce oxidative stress in the body—something that’s important for minimizing inflammation and supporting overall health. What’s more, research indicates that NAC may improve fertility outcomes for women with endometriosis, a major win if fertility is a concern. It’s like giving your body a reset button to help it function more efficiently and reduce the impact of oxidative damage.
• Magnesium Glycinate: Endometriosis can bring on cramping and muscle tension, but magnesium glycinate is here to help! Magnesium is known for its muscle-relaxing properties, making it perfect for relieving cramps and soothing discomfort. It’s also a sleep promoter, helping you unwind and get better rest—a key component of healing. Plus, magnesium can calm the nervous system, so you’re less likely to be overwhelmed by stress, which can make symptoms worse.
• Probiotics: Your gut is the epicenter of your health, and a healthy gut microbiome is essential for managing both hormone balance and inflammation. Probiotics can help by replenishing your beneficial gut bacteria, improving digestion, and even supporting your immune system. For those with endometriosis, a healthy gut may contribute to reduced systemic inflammation and better hormone regulation. To get the most out of probiotics, choose a multi-strain formula to ensure you’re covering all the bases.
While these supplements can be incredibly effective, remember that they’re not magic bullets—they’re just one part of the puzzle. Always consult with your healthcare provider before starting any new supplement regimen, so you can personalize your approach based on your unique needs. With the right guidance and the help of functional nutrition, you can take meaningful steps toward managing your endometriosis and improving your overall health.
It’s Not Just About Food: Lifestyle Matters
Managing endometriosis goes beyond meal plans and supplements; it’s about embracing the bigger picture, where everyday habits and choices play a crucial role. Stress, for example, is like a hidden villain—it ramps up inflammation and can make your symptoms even worse. So, let’s talk about ways to manage it!
Mindfulness practices and yoga are not just buzzwords; they’re powerful tools that can help reduce your stress levels, calm your nervous system, and lower overall inflammation. It’s amazing what a little breathing exercise or a gentle yoga flow can do for both your mind and body.
Don’t forget the power of rest! Skipping sleep is like ignoring your body’s recharge button. Getting enough high-quality sleep is essential for hormone regulation, tissue repair, and keeping your immune system in check. So, while you’re working on nourishing your body with food, make sure you’re nourishing your mind and taking time to recharge with some peaceful rest.
Real Talk: Why Personalization Is Key
When it comes to managing endometriosis, one size does NOT fit all. No two people experience the condition the same way, and that’s why a personalized approach is absolutely essential. Everyone has different triggers, so working with a dietitian or a functional medicine professional is key. They can help you pinpoint your unique triggers and craft a tailored plan that fits your lifestyle and needs. You might need to experiment with different foods, supplements, or lifestyle strategies to see what makes the biggest difference for you. The beauty of working with a pro is that they can provide you with the expertise and support to navigate this process and fine-tune your plan as you go along. It’s all about what works for YOU—not a generic, one-size-fits-all solution.
Wrapping It Up
Endometriosis doesn’t have to dictate your life. By embracing the principles of functional nutrition, you’re giving your body the tools it needs to fight back and thrive. Focus on anti-inflammatory foods, hormone balance, gut health, and tackling oxidative stress, and you’re already on the right path. But don’t forget that mindfulness, stress management, and quality sleep are just as important. Add in a dash of self-care and personalization, and you’ve got the perfect recipe for living your best life with endometriosis.
Sources:
https://pmc.ncbi.nlm.nih.gov/articles/PMC9983692
https://pmc.ncbi.nlm.nih.gov/articles/PMC8224039
https://www.rbmojournal.com/article/S1472-6483(13)00007-2/fulltext
https://pmc.ncbi.nlm.nih.gov/articles/PMC8065992
https://pmc.ncbi.nlm.nih.gov/articles/PMC7226034
https://drbrighten.com/causes-endometriosis-5-natural-treatment-strategies
https://drbrighten.com/endometriosis-relief-naturally
https://drbrighten.com/endometriosis-flare-up/#h-endometriosis-pain-control-nbsp
https://pmc.ncbi.nlm.nih.gov/articles/PMC9528818
https://pmc.ncbi.nlm.nih.gov/articles/PMC10058497/#sec5-life-13-00654

Hormonal fluctuations impact your energy levels, mood, and overall well-being throughout your menstrual cycle. By aligning your diet with these hormonal changes—a practice known as cycle syncing—you can optimize your energy, reduce PMS, and improve overall cycle health. This guide will help you understand the phases of the menstrual cycle and how nutrition can play a vital role in supporting hormonal balance.
Let’s begin by breaking down the menstrual cycle and understanding how your hormones fluctuate during each phase!
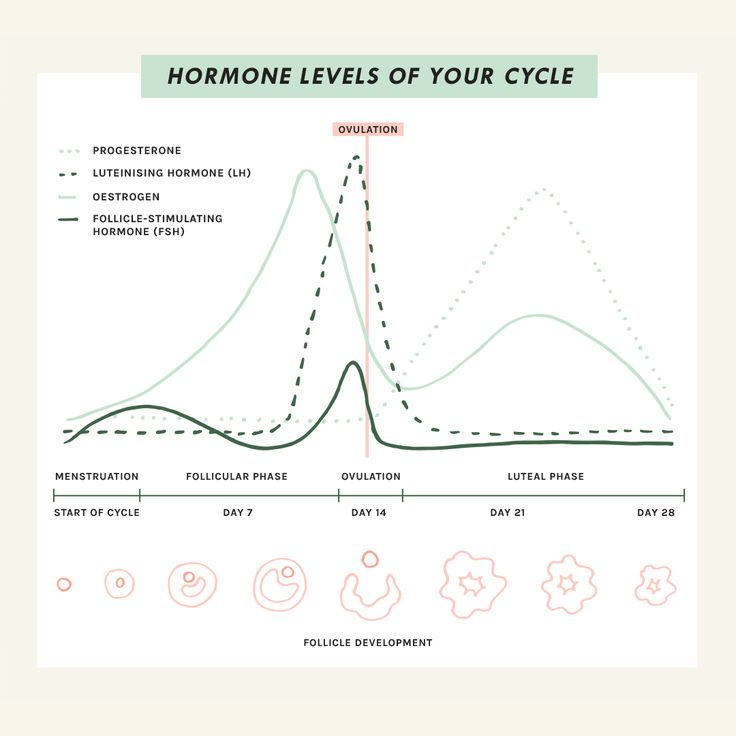
Phases of the Menstrual Cycle
The menstrual cycle has four distinct phases: the menstrual phase, follicular phase, ovulatory phase, and luteal phase. Each phase brings unique hormonal shifts that influence your body’s nutritional needs and energy requirements.
1. Menstrual Phase
(Day 1-6)
- This phase begins with menstruation. Hormone levels of estrogen and progesterone are at their lowest.
- Symptoms may include fatigue, cramping, and low energy levels.
2. Follicular Phase
(Day 7-13)
- Estrogen levels begin to rise, stimulating the growth of follicles in the ovaries and increasing energy.
- This is often when women feel their best, with improved mood and vitality.
3. Ovulatory Phase
(Day 14-16)
- Estrogen peaks, and luteinizing hormone (LH) surges to trigger ovulation.
- Energy levels and libido are typically at their highest.
4. Luteal Phase
(Day 17-28)
- Progesterone rises to prepare the uterus for a potential pregnancy, while estrogen levels dip. If fertilization does not occur, both hormones decrease, leading to PMS symptoms.
- Symptoms may include bloating, fatigue, and cravings.
Understanding these phases allows you to tailor your diet and lifestyle to support your body’s natural rhythms.
How Nutrition Supports Each Phase
Menstrual Phase: Focus on Iron and Hydration
During the menstrual phase, many individuals experience common symptoms such as cramping, fatigue, and irritability. While it may be tempting to indulge in comfort foods like sweets, pizza, and chips, these choices can disrupt hormonal balance and deplete important nutrients needed to support your body during this phase. Instead, focusing on nutrient-dense foods that support iron levels, reduce inflammation, and promote hydration. These all can help alleviate symptoms and maintain overall well-being.
- Foods to prioritize: One of the most important considerations during the menstrual phase is replenishing iron lost through bleeding. Incorporating iron-rich foods like lean red meat, spinach, lentils, beans, and beets can help restore iron levels. To optimize iron absorption, pair these foods with sources of vitamin C, such as citrus fruits, berries, broccoli, and bell peppers. Vitamin C enhances the bioavailability of iron, ensuring that your body can make the most of the iron you consume. Vitamin K is another key nutrient that can help reduce heavy bleeding. Leafy greens, blueberries, cheese, and eggs are excellent sources of vitamin K, which supports blood clotting and helps regulate menstrual flow. Omega-3 fatty acids are also beneficial during this phase, as they have anti-inflammatory properties that can help reduce cramping. Incorporate omega-3-rich foods like salmon, flaxseed, and tree nuts to support your body’s natural processes and ease discomfort.
- Hydration: This is particularly important during the menstrual phase, as it can help reduce bloating and prevent dehydration, which can exacerbate fatigue. Herbal teas such as ginger or chamomile are soothing options that can help alleviate cramps, reduce bloating, and promote relaxation.
- Avoid: Avoid high-sodium foods during your period, as they can exacerbate bloating and lead to water retention. Instead, focus on whole, nutrient-dense foods that provide essential vitamins and minerals, as well as plenty of hydration, to help you feel your best during this time.
Follicular Phase: Build Energy with Nutrient-Dense Foods
As estrogen rises, focus on foods that provide sustained energy and promote gut health. Maintaining gut health is deeply connected to hormonal balance, playing a crucial role in maintaining a healthy menstrual cycle. A well-functioning gut microbiome, particularly the estrobolome, aids in estrogen metabolism, preventing hormonal imbalances that could lead to PMS or heavy periods. Incorporating fiber-rich foods, probiotics, and fermented options can support gut health. These choices not only benefit your cycle but also improve digestion, energy, and mood, contributing to overall well-being!
- Foods to prioritize: Incorporate fiber-rich foods such as quinoa, oats, fresh vegetables, and seeds, which aid in digestion and promote stable blood sugar levels. Fermented foods like kimchi, sauerkraut, and yogurt are excellent choices as they provide beneficial probiotics that support gut health. Omega-3-rich foods like walnuts, chia seeds, and flaxseeds are also important as they have anti-inflammatory properties that can help balance hormones during this phase.
- Key nutrients: Prioritize B vitamins which support energy production and help combat fatigue, and omega-3 fatty acids, which promote overall hormonal balance and reduce inflammation.
- Avoid: It’s crucial to avoid refined sugars, as they can cause blood sugar spikes that disrupt energy levels and hormone regulation.
Ovulatory Phase: Support Detoxification
During the ovulatory phase, estrogen levels peak, and the body enters a high-energy phase, making it important to support both hormonal balance and overall vitality. Since the liver plays a key role in breaking down and detoxifying excess estrogen, it’s crucial to include foods that promote liver function and aid in estrogen metabolism.
- Foods to prioritize: Cruciferous vegetables (broccoli, kale, Brussels sprouts) are excellent choices, as they contain compounds such as sulforaphane that help the liver process estrogen more efficiently. Berries help reduce oxidative stress and inflammation, which can support overall hormonal health. Flaxseeds are also beneficial as they contain lignans that can bind to excess estrogen, helping to regulate levels in the body.
- Key nutrients: Zinc is a key nutrient for supporting ovulation, making it important to include zinc-rich foods like pumpkin seeds, shellfish, and legumes.
- Avoid: It’s important to avoid alcohol and excessive caffeine during this phase. Both substances can burden the liver, slowing down its detoxification processes and potentially causing hormonal imbalances. Drinking plenty of water and consuming foods rich in fiber will further support liver health and overall detoxification.
Luteal Phase: Balance Blood Sugar and Reduce Inflammation
Hormonal fluctuations, particularly increased progesterone, can contribute to common symptoms such as cravings, mood swings, fatigue, and bloating during this phase of your cycle. The key to managing these symptoms is balancing blood sugar levels, reducing inflammation, and nourishing your body with foods that support hormonal balance.
- Foods to prioritize: One effective strategy is to focus on complex carbohydrates, which provide steady energy and help stabilize blood sugar. Foods such as sweet potatoes, whole grains, and high-fiber vegetables, including cruciferous vegetables, can help curb hunger and keep blood sugar levels steady.
- Magnesium-rich foods are also important during this phase, as magnesium has been shown to alleviate PMS symptoms, including mood swings, irritability, and cramps. Magnesium-rich options like dark chocolate, almonds, and pumpkin seeds are excellent choices.
- Anti-inflammatory spices like turmeric and ginger can also be beneficial, as they help reduce inflammation, soothe cramps, and support overall well-being. These spices have natural properties that may help ease discomfort associated with PMS, including bloating and muscle tension.
- Key nutrients: Vitamin B6 is another important nutrient during the luteal phase, as it helps regulate mood and reduce irritability, which can be exacerbated by hormonal changes. Foods such as bananas, poultry, and potatoes are rich in vitamin B6 and can be incorporated into your meals to support emotional well-being during this time.
Avoid: If you’re craving something sweet or salty, opt for healthier alternatives such as dark chocolate, fruit, nuts, and seeds. These foods can satisfy cravings without causing the blood sugar spikes and crashes that processed snacks can induce. Additionally, staying hydrated is crucial during the luteal phase, as water helps reduce bloating, brain fog, and PMS-related discomfort.

Seed Cycling for Hormonal Balance
Seed cycling is a holistic dietary practice that involves eating specific seeds at different phases of the menstrual cycle to support hormone balance. The idea behind seed cycling is that different phases of the menstrual cycle require different hormone support, and specific seeds contain the nutrients necessary for this. This method is particularly beneficial for regulating irregular cycles and managing PMS symptoms.
Follicular Phase (Day 1-14)
During the follicular phase, estrogen is the dominant hormone. The goal is to support estrogen production and metabolism. The recommended seeds for this phase are raw, freshly ground flaxseeds and pumpkin seeds. Flaxseeds are rich in lignans, which have weak estrogenic properties and support elimination. Pumpkin seeds, on the other hand, provide zinc, an essential mineral for testosterone production and healthy hormone levels.
- Seeds: Flaxseeds and pumpkin seeds
- Benefits: Flaxseeds contain lignans that help balance estrogen levels. Pumpkin seeds provide zinc to support progesterone production later in the cycle.
Luteal Phase (Day 15-28)
After ovulation, progesterone becomes the dominant hormone. To support this, the recommended seeds are raw, freshly ground sunflower seeds and sesame seeds. Sunflower seeds are rich in vitamin E, which helps reduce PMS symptoms and supports estrogen detoxification. Sesame seeds are high in lignans and fatty acids, which help balance progesterone and reduce inflammation.
- Seeds: Sesame seeds and sunflower seeds
- Benefits: Sesame seeds contain lignans to modulate estrogen, and sunflower seeds provide selenium to support liver detoxification.
Can Seed Cycling Be Used Mid-Cycle? Yes, seed cycling can be started at any point in the cycle, depending on where you are in your menstrual phase. If you’re tracking your cycle closely, you can adjust your seed rotation accordingly to match your ovulation timing.
Seed Cycling’s Nutritional Basis The seeds used in seed cycling are rich in essential nutrients that support hormone production, including omega-3 fatty acids, zinc, magnesium, and antioxidants. These nutrients help optimize hormone balance by supporting estrogen and progesterone levels, promoting healthy testosterone levels, and reducing inflammation, which can lead to hormonal imbalances.
Seed Cycling Science Although the term “seed cycling” itself is not widely researched in scientific literature, the individual nutrients in the seeds have been extensively studied for their health benefits. For example, lignans in flaxseeds have been linked to improved estrogen and progesterone balance, and the zinc in pumpkin seeds supports testosterone production. Research has also shown that these seeds can benefit cardiovascular health, gut health, and even cancer prevention.
Does Seed Cycling Really Work? While more research is needed to fully validate seed cycling as a hormone-balancing practice, many women have reported positive changes in their menstrual health, including improved hormone balance, reduced PMS symptoms, and better skin health. The key is consistency and combining seed cycling with other healthy lifestyle practices, such as a balanced diet, adequate sleep, and stress management.
Additional Benefits of Seed Cycling
- For Menopause: Seed cycling can be continued post-menopause by aligning the seed rotation with the moon cycle. This can help manage symptoms like hot flashes and mood swings.
- For PCOS: Seed cycling can help balance testosterone and estrogen levels in women with PCOS, potentially alleviating symptoms like acne and hirsutism.
- For Acne: Seed cycling may help improve acne by balancing hormones, particularly when coming off hormonal birth control, which can trigger an androgen rebound and worsen acne.
- For Painful Periods: Seed cycling may help reduce period pain by balancing estrogen and progesterone levels and supporting inflammation reduction.
How to Start Seed Cycling To begin seed cycling, it’s recommended to consume 1-2 tablespoons of freshly ground, raw seeds daily. You can add them to smoothies, salads, oatmeal, or even make homemade seed-based snacks! Consistency is key, and it’s best to give the practice at least one full cycle (about a month) to assess its effectiveness.
Exercise and Cycle Syncing
Adjusting your exercise routine to match your cycle phases can optimize performance and reduce hormonal stress.
- Menstrual Phase: Prioritize rest and gentle movements like yoga or walking.
- During your period, light activities like walking, stretching, or gentle movement can help ease discomfort and match your energy levels, especially if you’re dealing with cramps.
- While it’s natural to feel less active on the first day of your period, exercise can actually relieve cramps, boost energy, and improve your mood! Surprisingly, even in the early follicular phase, you might find you can lift heavier weights or handle more intense workouts. The key is to listen to your body and adjust your activity based on how you feel rather than sticking to rigid rules or expectations.
- Follicular Phase: Increase intensity with strength training and cardio as energy levels rise.
- During this phase of your cycle, rising estrogen and testosterone levels can enhance muscle-building potential, making cardio and strength training feel more effective. By as early as day three of your period, you might notice a boost in energy and exercise stamina as estrogen levels continue to climb!
- Ovulatory Phase: Engage in high-intensity workouts like HIIT or running.
- This typically occurs between the end of week two and the start of week three in your cycle and can leave you feeling more energized. During this time, many women notice they can handle higher levels of physical exertion compared to other phases.
- Luteal Phase: Shift to moderate-intensity exercises like Pilates or swimming to accommodate fatigue.
- After ovulation, some women notice a quick drop in exercise tolerance, while others experience this closer to their period. The week before your period can bring challenges like reduced tolerance, trouble cooling down, and water retention, which may affect workouts. Staying hydrated, focusing on electrolytes, wearing breathable clothing, and exercising in a cool space can help. This is a great time to prioritize recovery with activities like yoga or Pilates.
- Increased hunger is normal due to higher calorie needs, especially carbohydrates, as your body becomes less insulin sensitive. You can honor your cravings or increase your intake by 5–10%, choosing what works best for you!
This cyclical approach helps prevent overtraining and supports hormonal balance.
Lifestyle Tips for Cycle Health
- Stress Management: Chronic stress can disrupt hormonal balance. Incorporate mindfulness practices like meditation or journaling.
- Adequate Sleep: Aim for 7-9 hours per night to support hormone production and recovery.
- Track Your Cycle: Use apps or journals to monitor your symptoms and identify patterns.
Conclusion
Cycle syncing empowers you to take control of your health by aligning nutrition, exercise, and lifestyle with your menstrual cycle! By nourishing your body with the right foods at the right time, you can alleviate symptoms, enhance energy levels, and promote overall well-being. Implementing practices like seed cycling and phase-specific exercise further supports hormonal harmony.
Start small and make gradual changes to experience the benefits of cycle syncing. Your body will thank you for it!
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC10251302
https://www.ncbi.nlm.nih.gov/search/research-news/17857
https://health.clevelandclinic.org/nutrition-and-exercise-throughout-your-menstrual-cycle
https://drbrighten.com/how-to-exercise-with-your-cycle
https://drbrighten.com/seed-cycling-for-hormone-balance
https://drbrighten.com/seed-cycling-menopausal-hormones
https://drbrighten.com/gut-hormone-connection
Images
Female Cycle https://www.pinterest.com/pin/962222276632847842/
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook