Registered dietitian, functional nutritionist, & your new fertility BFF. I'm passionate about helping women thrive during preconception, pregnancy, and postpartum.
Nutrition
PCOS
Fertility
View All
Explore the blog
Hi, I'm Anabelle
Non-toxic Living
Work with our team
Digging Deep: Understanding the Root Causes of Recurrent Pregnancy Loss
Introduction to Recurrent Pregnancy Loss
Facing recurrent pregnancy loss (RPL) can be both emotionally and physically draining. Defined by the American Society for Reproductive Medicine (ASRM) as two or more consecutive pregnancy losses, RPL affects approximately 1-2% of couples trying to conceive. Traditionally, it was defined as three or more losses, but recent guidelines from the European Society of Human Reproduction and Embryology (ESHRE) have adopted the more inclusive definition.
Understanding the root causes of RPL is essential for finding effective treatments and support. The journey often involves a multitude of factors, from genetic anomalies to hormonal imbalances, and even infections. Although the causes can be complex, advancements in research and technology offer hope for affected couples.
Our goal here is to explore various underlying reasons behind RPL, the diagnostic tests available, and the emerging treatments promising to make an impact. Whether you’re experiencing this challenging condition or supporting someone who is, this guide aims to provide the information needed for a proactive approach to managing recurrent pregnancy loss.

Genetic Factors Behind Recurrent Pregnancy Loss
When it comes to recurrent pregnancy loss (RPL), genetics play a pivotal role. Chromosomal anomalies, whether in the parents or the embryo, contribute significantly to this heart-wrenching condition. A karyotype analysis, which examines the number and structure of chromosomes, is often recommended for both partners to identify any genetic irregularities. Coupled with other diagnostic tests, this can uncover potential genetic causes behind RPL.
Most pregnancy losses occur due to random chromosomal abnormalities, such as aneuploidy, which is the presence of an abnormal number of chromosomes in a cell. These anomalies often happen spontaneously and are not typically inherited. However, certain genetic defects in either parent can increase the risk of such random events. If a parent is a carrier of a balanced translocation, for instance, it can lead to unbalanced translocations in the embryo, resulting in miscarriage.
An emerging field of study is the role of single nucleotide polymorphisms (SNPs) in pregnancy loss. SNPs are variations in a single nucleotide that occur at a specific position in the genome. While the impact of SNPs is still under investigation, some have been linked to reproductive issues, providing another layer of complexity to the genetic factors involved in RPL.
Knowing these factors allows for tailored approaches when considering future pregnancies. Genetic counseling is often recommended to help couples understand their risk and explore reproductive options. For some, preimplantation genetic testing (PGT) during in vitro fertilization (IVF) might be a viable option, as it allows for the selection of embryos without specific genetic anomalies.
Understanding the genetic basis of recurrent pregnancy loss is fundamental. By addressing these factors, couples can be better prepared and supported in their journey toward a successful pregnancy.
Hormonal Imbalances: A Hidden Culprit
Hormonal imbalances are often overlooked yet significant contributors to recurrent pregnancy loss (RPL). Common endocrine disorders, such as thyroid disease and diabetes, can profoundly impact pregnancy viability. For instance, hypothyroidism, a condition where the thyroid gland does not produce sufficient hormones, can disrupt the delicate hormonal balance required for a successful pregnancy. Similarly, uncontrolled diabetes can lead to poor blood sugar control, which adversely affects fetal development.
Another frequent hormonal imbalance involves the levels of progesterone, a hormone crucial for maintaining the uterine lining during pregnancy. Insufficient progesterone can result in the uterine lining shedding prematurely, leading to miscarriage. Hormonal fluctuations brought about by polycystic ovary syndrome (PCOS) can also elevate the risk of pregnancy complications, as the condition often results in irregular ovulation and associated hormonal imbalances.
Addressing these hidden culprits requires a proactive approach. Comprehensive hormonal screenings and timely interventions can help regulate these imbalances. Potential treatments might include thyroid hormone replacement therapy, insulin management for diabetes, and progesterone supplementation. By stabilizing these hormonal levels, it’s possible to create a more conducive environment for pregnancy, substantially reducing the risk of RPL.
It’s essential to discuss any symptoms or concerns with your healthcare provider. Identifying and managing hormonal issues early can offer hope and improve outcomes for those affected by recurrent pregnancy loss.
Genetic Factors Behind Recurrent Pregnancy Loss
When delving into the genetic factors behind recurrent pregnancy loss (RPL), it becomes evident that variations in chromosomes are often to blame. Around half of first-trimester miscarriages are linked to chromosomal abnormalities, such as aneuploidy – the gain or loss of one or more chromosomes. These abnormalities can result in conditions like Turner syndrome and Down syndrome, leading to pregnancy loss.
Additionally, structural chromosomal rearrangements, including translocations and inversions, can also contribute to RPL. In such cases, the parents may carry balanced rearrangements that go unnoticed until they attempt to conceive, only to result in recurrent miscarriages. Karyotype analysis of both partners can help in detecting these chromosomal issues, allowing for an informed approach to treatment or reproductive alternatives like IVF with preimplantation genetic testing.
The genetic architecture of sporadic versus recurrent miscarriage also shows marked differences. While a single miscarriage might be attributed to sporadic genetic mutations, recurrent miscarriages often indicate a deeper genetic predisposition. Recent research involving genome-wide scans in sibling pairs with idiopathic recurrent miscarriage has revealed genetic linkages, suggesting a hereditary component that warrants further investigation.
Moreover, advanced maternal age is a significant factor contributing to genetic anomalies. Women over 35 years old face a higher risk of chromosomal aberrations in their ova, increasing the likelihood of recurrent pregnancy loss. With age, the quality and genetic integrity of a woman’s eggs decline, resulting in a higher probability of abnormal embryonic development.
Ultimately, understanding the genetic factors involved in RPL is crucial for developing targeted interventions. While genetic counseling and testing are fundamental tools, ongoing research and emerging technologies are continually improving our ability to diagnose and manage these complex genetic issues.
The Role of Infections in Recurrent Pregnancy Loss
While the role of infection in first-trimester recurrent pregnancy loss (RPL) remains somewhat ambiguous, it’s a factor that cannot be entirely ruled out. Infectious agents might contribute to pregnancy loss if they establish a persistent presence in the reproductive tract. Some studies suggest infections, particularly chronic or undetected, could disrupt the delicate balance necessary for a successful pregnancy.
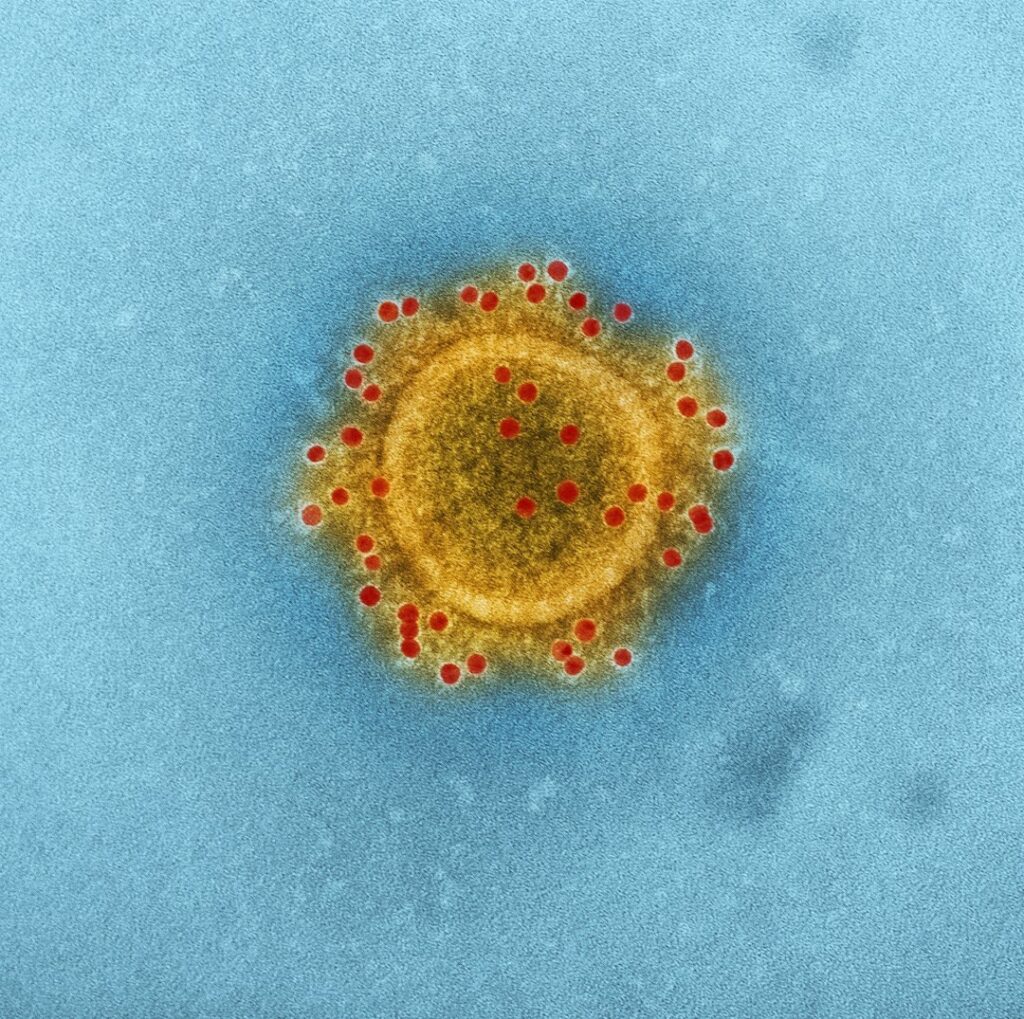
Bacterial vaginosis, for example, has been associated with adverse pregnancy outcomes, including RPL. Similarly, certain viral infections like cytomegalovirus (CMV) and herpes simplex virus (HSV) have been explored in connection with pregnancy complications. However, the exact mechanisms by which these infections might lead to recurrent losses are not fully understood and require more in-depth research.
Furthermore, infections that trigger an inflammatory response can be particularly problematic. Inflammation can impair implantation or placental development, both crucial for sustaining a pregnancy. Therefore, a thorough evaluation for infections may be a necessary step in identifying the root causes of unexplained RPL.
At times, treating an underlying infection can improve pregnancy outcomes. For instance, antibiotics may be prescribed if a bacterial infection is detected. However, the decision to treat depends on a comprehensive diagnosis and understanding of the specific infections involved.
In conclusion, while infections are a potential factor in RPL, the challenge remains in their identification and the understanding of their exact impact. Future research focusing on the relationship between infectious agents and pregnancy loss could offer deeper insights and pave the way for more effective management strategies.
Autoimmune Disorders and Pregnancy Loss
Autoimmune disorders play a critical role in recurrent pregnancy loss (RPL). These disorders occur when the body’s immune system mistakenly attacks its own tissues. In the case of pregnancy, sometimes the immune system may target the placenta or developing embryo, leading to complications.
A prominent example of this is Antiphospholipid Syndrome (APS). This condition is characterized by the presence of antiphospholipid antibodies, such as anticardiolipin and lupus anticoagulant, which can interfere with normal blood clotting and contribute to pregnancy loss. Early miscarriage, stillbirth, and other pregnancy complications are often linked to APS. If you have a history of autoimmune disorders, discussing APS testing with your healthcare provider is crucial for a thorough evaluation.
Another autoimmune factor to consider is the role of anti-inflammatory cytokines. These specialized proteins are part of the body’s immune response and can be produced by placental and decidual tissues. However, an overproduction may result in inflammation, disrupting the environment necessary for a successful pregnancy.
Research and updated 2023 ESHRE guidelines have pointed out the importance of scrutinizing autoimmune factors in recurrent pregnancy loss. Diagnostic tests often focus on identifying these antibodies and assessing immune function. It’s worth noting that early and accurate diagnosis can significantly improve management and treatment options, increasing the chances of a successful pregnancy.
Understanding how autoimmune disorders contribute to recurrent pregnancy loss underscores the importance of a holistic approach to diagnosis and treatment. By addressing these underlying issues, healthcare providers can offer more personalized and effective care plans, ultimately supporting a healthier pregnancy journey for those affected by RPL.
Diagnostic Tests for Uncovering Root Causes

Getting to the bottom of recurrent pregnancy loss involves a comprehensive and often multifaceted approach. The first step typically involves a detailed medical history and physical examination. This initial evaluation can offer vital clues and help in tailoring further testing.
Beyond the basics, specialized tests are essential for identifying the underlying causes. Blood tests can reveal hormonal imbalances by measuring levels of thyroid-stimulating hormone (TSH) and prolactin, which play critical roles in maintaining a healthy pregnancy. Similarly, antiphospholipid antibody (APA) and thrombophilia testing can detect autoimmune disorders that might contribute to pregnancy loss.
Genetic testing is another crucial component. Karyotype analysis of both partners can identify chromosomal abnormalities that might be a significant cause of recurrent pregnancy loss. In some cases, cytogenetic testing of the pregnancy tissue itself is performed to look for abnormalities in the fetus.
Some studies suggest testing for Factor V Leiden (FVL) mutations, especially in cases of unexplained or idiopathic early recurrent pregnancy loss. Though not always conclusive, such tests can provide invaluable information for managing the condition.
Imaging studies also play a vital role. Ultrasound (US) examinations or histopathologic evaluations of the uterine cavity can identify structural abnormalities like fibroids or a septate uterus, which might hinder a successful pregnancy.
Ultimately, the goal is to identify modifiable etiological and risk factors for effective treatment. By combining detailed medical history, specialized blood tests, genetic testing, and imaging studies, you and your healthcare provider can develop a personalized strategy aimed at overcoming recurrent pregnancy loss.
| Study | Year | Factor Investigated | Impact on Recurrent Pregnancy Loss |
| Evans, J. et al. | 2018 | Genetic Factors | Significant |
| Johnson, R. et al. | 2017 | Hormonal Imbalances | Moderate to High |
| Smith, A. et al. | 2019 | Infections | Low to Moderate |
| Lee, C. et al. | 2020 | Autoimmune Disorders | High |
Identifying the Root Causes of Recurrent Pregnancy Loss
When it comes to recurrent pregnancy loss (RPL), identifying the root causes is crucial. The complexity of RPL means that it often results from a multifactorial interplay of genetic, hormonal, anatomical, and immunological factors. Each potential cause warrants careful investigation and testing to develop an effective management plan.
Genetic Factors: Chromosomal abnormalities are a common cause of RPL. A detailed medical history and karyotype analysis of both partners can reveal genetic irregularities. Advanced techniques like a 24-chromosome microarray analysis of miscarriage tissue have shown to determine a probable or definite cause in over 90% of cases.
Hormonal Imbalances: Hormonal issues, such as thyroid disorders, polycystic ovary syndrome (PCOS), or luteal phase insufficiency, can significantly impact pregnancy viability. Blood tests and hormonal profiling help in detecting these imbalances, allowing for targeted treatments.
Anatomical Abnormalities: Uterine anomalies like septate uterus, fibroids, or adhesions can prevent the proper implantation and growth of the embryo. Imaging techniques, such as hysterosonography or MRI, can identify these structural issues. Surgical interventions often correct them, improving pregnancy outcomes.
Immunological Factors: Autoimmune disorders, where the body’s immune system mistakenly attacks its own tissues, can also play a role. Conditions like antiphospholipid syndrome (APS) need specific blood tests and expert evaluation for a definitive diagnosis, followed by immune-modulating therapies.
Infections: Certain infections can disrupt the delicate environment of the uterus, leading to pregnancy loss. Screening for infections and appropriate treatments are vital, especially if there’s a history suggestive of infectious agents.
Understanding these potential causes, through a combination of detailed medical history, meticulous physical examination, and a spectrum of diagnostic tests, is key in offering hope and tailored treatments to women struggling with recurrent pregnancy loss.
Future Research and Emerging Treatments
As we look ahead, the field of recurrent pregnancy loss (RPL) is evolving with promising avenues of research and innovative treatments. One particularly exciting area is the use of next-generation sequencing (NGS). This technology allows for an in-depth examination of genetic factors that may contribute to RPL, offering more personalized and targeted approaches to treatment. By pinpointing specific genetic anomalies, clinicians can tailor interventions to the individual needs of each couple, potentially improving outcomes significantly. Additionally, there’s a growing recognition of the importance of addressing the psychosocial needs of couples dealing with RPL. Future studies and treatment plans are increasingly incorporating mental health support as a crucial component. This holistic approach not only aims to improve emotional well-being but also to provide comprehensive care that addresses both physical and psychological factors of pregnancy loss.
While various treatments are currently available, there is no one-size-fits-all solution. This is where more extensive randomized controlled trials (RCTs) come into play. There is a pressing need for larger and more rigorous trials, ideally conducted across multiple centers, to evaluate the efficacy of different surgical procedures and medical treatments. Such research efforts would provide clearer guidelines and more effective management strategies for RPL.
Current meta-analyses often consider a diverse array of patient populations and treatment methodologies, resulting in inconsistent recommendations. Therefore, future analyses must focus on more homogenous patient groups to derive more applicable and precise conclusions. By refining the subsets of patients studied, we can ensure that the resulting data is both relevant and practical for specific demographics.
Another crucial aspect is the development of improved prognostic tools. These tools aim to predict the likelihood of pregnancy loss recurrence, empowering healthcare providers to devise more effective, customized treatment plans. This predictive capability is vital in managing expectations and creating proactive medical strategies for couples at risk.
Ultimately, the goal is to enhance our understanding of the modifiable etiological and risk factors associated with RPL. By identifying and addressing these factors, treatment strategies can become more effective, leading to better outcomes for those affected. As research progresses, the hope is that emerging treatments and interventions will offer new hope and possibilities for couples experiencing recurrent pregnancy loss.
Getting Support
If you’re looking for more support on your fertility journey, utilizing functional nutrition, you can apply to work with our team of dedicated fertility dietitians here.
Leave a Reply Cancel reply
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook
Functional nutrition for women & couples trying to conceive
Get the Preconception Playbook
Actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.

I never thought I would be herpes negative again, after been diagnosed for 4 years, I have tried everything possible in life, from one medical doctor to another, one hospital to another, series of tests, different kinds of medication, I had already lost hope until I meet Great Dr. Riaria online testimonies, a specialist in herbal medication from Africa, I contacted him through his email and number I got from one of the many testifiers, and he prepared herpes herbal medication for me which I took for weeks and now I am completely cured. I have gone to different hospitals for check ups to be totally sure, and all my results are negative. I want to use this medium to express my gratitude to him for saving my life and curing me from herpes virus, for taking away all my pains and sorrows, I’m indeed grateful and I am so happy I’m now herpes negative. I will continue to tell the good news of your great works to everyone. drriaria@gmail. com