Resources
Style
Planning
View All
THE blog
Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Hormonal contraceptives, including birth control pills, patches, injections, and intrauterine devices (IUDs), have transformed reproductive health, offering women reliable family planning options. However, many individuals experience symptoms after discontinuing hormonal contraception, a phenomenon sometimes referred to as post-birth control syndrome (PBCS). These symptoms can range from irregular cycles and acne to mood swings and digestive issues. Understanding the impact of hormonal contraceptives on the body and implementing strategies to support recovery can help ease this transition.
Understanding the Effects of Hormonal Contraceptives
Hormonal contraceptives work by suppressing ovulation, altering cervical mucus, and changing the uterine lining to prevent pregnancy. While effective, these changes influence several body systems, including the endocrine, digestive, and immune systems. Long-term use can disrupt the body’s natural hormone production, leading to potential withdrawal effects when stopping contraception.
A recent study found that hormonal contraceptives impact the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress response and hormone production. This may explain why some women experience mood disturbances and fatigue after discontinuation. Additionally, research suggests that birth control pills may alter gut microbiota composition, contributing to inflammation and digestive issues post-contraception.
The Role of the HPA Axis
The HPA axis plays a crucial role in regulating cortisol, a stress hormone that influences metabolism, immune function, and mood. Studies have shown that long-term contraceptive use can disrupt this delicate balance, leading to post-pill anxiety, fatigue, and even adrenal dysfunction. As the body readjusts, individuals may experience heightened stress sensitivity and emotional imbalances.
Additionally, research suggests that chronic hormonal suppression can contribute to reduced ovarian hormone production post-contraception, leading to symptoms like irregular cycles, low libido, and difficulty ovulating.
Common Symptoms After Stopping Hormonal Contraceptives
Post-birth control syndrome encompasses a variety of symptoms that may arise within weeks or months after stopping contraception.
Common symptoms include:
- Irregular or absent menstrual cycles
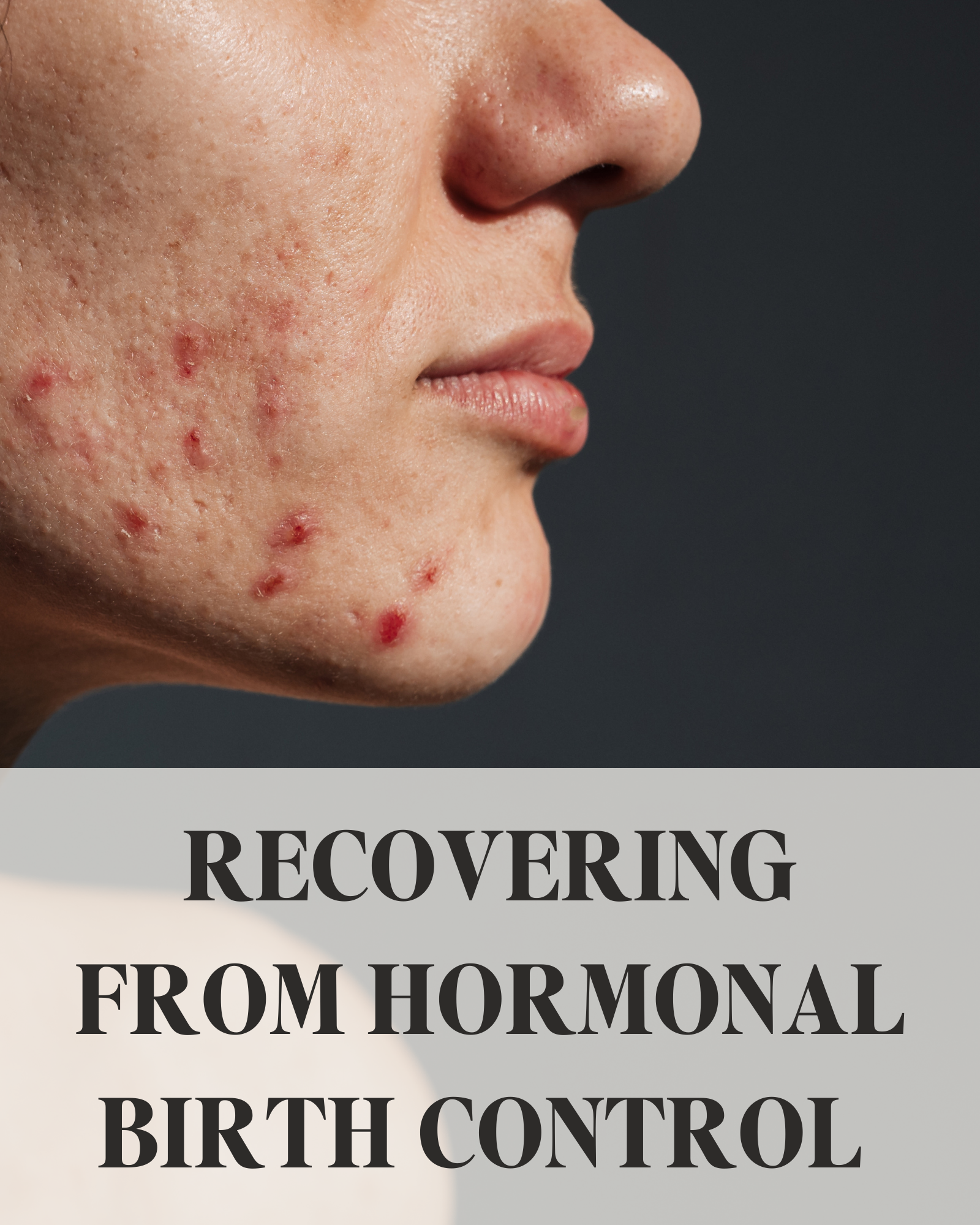
- Acne and skin changes
- Hair loss or thinning
- Digestive disturbances, including bloating and constipation
- Fatigue and mood swings
- Low libido
- Headaches and joint pain
These symptoms occur as the body attempts to restore natural hormone balance. For some, this transition is seamless, while for others, it may take several months to regulate.
Life After Birth Control: What to Expect
The transition off hormonal contraceptives varies for each individual. Some experience a smooth adjustment, while others face lingering hormonal imbalances.
- Menstrual Cycle Irregularities: It may take several months for cycles to regulate. If cycles remain absent or irregular for more than six months, professional evaluation is recommended. Ovulatory dysfunction is common post-contraception, particularly after long-term use of hormonal birth control. Tracking basal body temperature (BBT) and cervical mucus can provide insight into ovulation status and cycle health
- Acne and Skin Changes: Hormonal shifts can temporarily worsen acne. Supporting detox pathways, reducing dairy and sugar intake, and using non-comedogenic skincare products can help. Elevated androgens post-pill can contribute to excess sebum production, leading to breakouts. Incorporating zinc, omega-3 fatty acids, and antioxidants may promote clearer skin.
- Mood and Energy Levels: Some experience heightened anxiety or depression post-contraception. Prioritizing gut health, sleep, and stress reduction can ease this transition. The gut-brain axis plays a key role in mood regulation, making probiotics and a fiber-rich diet beneficial for mental well-being.
- Fertility Awareness: Some individuals regain fertility immediately, while others need time for ovulation to resume. Those trying to conceive may benefit from monitoring ovulation signs. If fertility does not return within six months, an evaluation for conditions like post-pill PCOS or hypothalamic amenorrhea may be necessary.
- Weight Fluctuations: Water retention and metabolism changes can impact weight. Focusing on whole foods, movement, and hydration supports a stable transition. Hormonal contraceptives can affect insulin sensitivity, and some women notice changes in blood sugar regulation post-pill. Balancing macronutrients and avoiding refined sugars can help stabilize weight.
- Increased Libido: Many report improved libido and natural cycle awareness after stopping hormonal contraceptives due to restored testosterone and estrogen levels.
Adjusting to life after birth control involves patience and self-care. Tracking symptoms, optimizing nutrition, and seeking support when needed can help individuals regain hormonal balance and overall well-being.
Supporting Hormonal Balance Post-Contraception
While post-birth control symptoms can be challenging, several strategies can support the body’s recovery and restore hormonal balance.
1. Nourishing Your Body with Key Nutrients
Hormonal contraceptives can deplete essential nutrients, including B vitamins, magnesium, zinc, and vitamin C. It has been found essential to replenish these nutrients to support metabolism, immune function, and hormone production.
Incorporating the following nutrient-dense foods can be beneficial:
- B Vitamins: Found in leafy greens, eggs, and whole grains
- Magnesium: Present in nuts, seeds, and dark chocolate
- Zinc: Found in oysters, beef, and lentils
- Vitamin C: Abundant in citrus fruits, bell peppers, and strawberries
Supplementing with a high-quality multivitamin or targeted nutrients may also help restore levels more efficiently.
2. Prioritizing Liver Health
The liver plays a crucial role in metabolizing hormones and detoxifying excess estrogen. Supporting liver function can aid hormone clearance and balance. Key strategies include:
- Drinking plenty of water to support detoxification
- Eating cruciferous vegetables (broccoli, cauliflower, kale) to promote estrogen metabolism
- Avoiding alcohol and excessive caffeine, which can burden the liver
- Taking liver-supporting supplements such as milk thistle and dandelion root
3. Balancing Blood Sugar Levels
Insulin resistance and blood sugar imbalances can contribute to hormonal dysregulation post-contraception. Stabilizing blood sugar helps maintain steady energy levels and prevents cortisol spikes, which can further disrupt hormones. To support blood sugar balance:
- Consume protein and healthy fats with every meal
- Avoid refined carbohydrates and excessive sugar
- Incorporate fiber-rich foods, such as legumes, nuts, and vegetables
- Engage in regular physical activity to improve insulin sensitivity
4. Restoring Gut Health
The gut microbiome influences hormone metabolism and immune function. Studies suggest that hormonal contraceptives may alter gut bacteria, leading to digestive issues and inflammation. Supporting gut health can enhance nutrient absorption and hormone clearance:
- Probiotic-Rich Foods: Yogurt, kimchi, sauerkraut, and kefir can replenish beneficial bacteria
- Prebiotic Fiber: Found in onions, garlic, bananas, and asparagus to support microbial diversity
- Bone Broth and Collagen: Aid in gut lining repair
- Limiting Processed Foods: Reducing inflammatory foods can alleviate digestive distress
- Fermented Foods and Fiber: Incorporating fermented foods like miso and fiber-rich foods such as flaxseeds can further support microbiome diversity
According to research, discontinuing birth control can cause shifts in the gut microbiome that affect estrogen metabolism and immune responses. A focus on gut healing post-contraception may accelerate hormonal recovery and reduce systemic inflammation.
5. Managing Stress and Prioritizing Sleep
Chronic stress and inadequate sleep can exacerbate hormonal imbalances. Since the HPA axis is affected by hormonal contraceptives, post-contraceptive recovery requires stress management techniques. Effective strategies include:
- Practicing mindfulness or meditation
- Engaging in gentle movement, such as yoga or walking
- Setting a consistent sleep schedule and avoiding blue light before bedtime
- Taking adaptogenic herbs, like ashwagandha or rhodiola, to support adrenal function
6. Tracking Your Menstrual Cycle
Monitoring menstrual patterns post-contraception provides insight into hormonal recovery. Using a cycle-tracking app or basal body temperature charting can help identify ovulation and cycle health.
- Basal Body Temperature (BBT): Measuring BBT each morning helps detect ovulation. A sustained temperature rise typically indicates ovulation has occurred.
- Cervical Mucus Changes: Observing cervical mucus consistency can signal fertility. Egg-white-like mucus usually indicates peak fertility.
- Cycle Length and Symptoms: Keeping track of cycle length, PMS symptoms, and flow characteristics provides valuable data about hormonal balance.
- Ovulation Predictor Kits: These kits measure luteinizing hormone (LH) surges, indicating the fertile window.
If menstruation does not return within three to six months, consulting a healthcare provider may be necessary to rule out underlying conditions like hypothalamic amenorrhea or PCOS.
7. Seeking Professional Support
If symptoms persist or become severe, working with a healthcare provider, such as a functional medicine/nutrition practitioner, can be beneficial. They can assess hormone levels, address underlying imbalances, and provide personalized recommendations for recovery.
Here are some issues you may need to address:
Prolonged Absence of Periods: If your period hasn’t returned after six months.
Persistent Acne or Severe Hair Loss: Significant changes in skin or hair health could indicate hormonal imbalances that require attention.
Excessive Mood Changes or Fatigue: If symptoms like mood swings, anxiety, or extreme tiredness persist.
Chronic Digestive Issues: Ongoing digestive disturbances such as bloating or constipation.
Conclusion
Recovering from hormonal contraceptives is a unique process for every individual. While some may transition smoothly, others may experience a range of symptoms as their body readjusts. By focusing on nutrient replenishment, liver and gut health, blood sugar balance, stress management, and cycle tracking, individuals can support their hormonal recovery more effectively. If challenges persist, seeking professional guidance can ensure a smoother transition and optimal long-term health.

Sources:
https://drbrighten.com/post-birth-control-syndrome
https://drbrighten.com/stopping-birth-control-side-effects
https://www.sciencedirect.com/science/article/pii/S0889159123003331?via%3Dihub
https://pmc.ncbi.nlm.nih.gov/articles/PMC6055351
https://drbrighten.com/the-contraception-guide/ https://www.kernodle.com/obgyn_blog/side-effects-of-stopping-the-pill-after-prolonged-use/
Many women with PCOS struggle to find an effective treatment plan due to its complex nature. However, recent research has begun to shine a light on the crucial role the gut microbiome plays in managing this condition. Your gut does more than just digest food; it influences hormone regulation, inflammation, and even your overall metabolic health.
This article dives into how optimizing your gut health can significantly impact PCOS management. From understanding the gut-hormone link to practical dietary changes you can make, you’ll gain valuable insights to improve your wellbeing.
Understanding PCOS: A Brief Overview
Polycystic Ovary Syndrome (PCOS) affects a significant portion of women around the world, with implications that go beyond just the reproductive system. At its core, PCOS is a hormonal disorder known for causing irregular menstrual cycles, excess androgen levels, and polycystic ovaries. But, it doesn’t stop there. This complex condition often brings a host of other challenges, including insulin resistance, obesity, type 2 diabetes, and cardiovascular issues.
The exact cause of PCOS remains a subject of ongoing research, but genetics and lifestyle factors both appear to play substantial roles. Women with PCOS frequently exhibit elevated insulin levels, which can exacerbate symptoms and contribute to the imbalance of sex hormones. What’s more, the syndrome can profoundly impact mental health, leading to conditions like anxiety and depression.
With no known cure, managing PCOS involves a combination of lifestyle modifications, dietary adjustments, and medical treatments tailored to alleviate specific symptoms. Because PCOS affects different women in different ways, it’s crucial to approach treatment on an individualized basis. In recent years, emerging studies have started to explore the connection between gut health and PCOS, revealing that a balanced gut microbiome might be an essential key to managing this disorder.

The Gut-Health Connection: Why It Matters
Your gut health doesn’t just affect your digestion; it has a profound impact on your overall well-being. The human gut microbiome, an ecosystem of trillions of bacteria, fungi, and other microorganisms, plays a crucial role in many bodily functions. Notably, it helps regulate metabolism, supports the immune system, and maintains the structural integrity of the gut lining.
But the relationship between gut health and conditions like Polycystic Ovary Syndrome (PCOS) is particularly interesting. The gut-brain axis, a complex communication network that links your gut and brain, further illustrates this connection. When your gut microbiota is in balance, it positively influences hormonal health, which is central to managing PCOS symptoms.
Emerging research highlights how an imbalance in the gut microbiota, also known as dysbiosis, can exacerbate PCOS symptoms. Dysbiosis has been linked to increased inflammation, insulin resistance, and hormonal imbalances—all of which are critical factors in PCOS. This makes maintaining a healthy gut not just a recommendation, but a necessity for those managing PCOS.
Moreover, factors like diet, sleep, and exercise play a significant role in shaping your gut microbiome. Consuming a diet rich in diverse, fiber-rich foods, getting quality sleep, limiting alcohol intake, and engaging in regular physical activity can all foster a healthier gut. By focusing on these areas, you can support your gut health and, in turn, help manage PCOS more effectively.
How Gut Bacteria Influence Hormonal Balance
In understanding gut health’s role in PCOS, it’s essential to dive into the relationship between gut bacteria and inflammation. Gut microbiota plays a crucial role in regulating hormones and metabolism. When your gut microbiota is unbalanced, it can lead to chronic inflammation, a common issue in those with PCOS. But how exactly does this happen?
Your gut lining serves as a barrier, preventing harmful substances from entering your bloodstream. However, an imbalanced gut microbiota can weaken this barrier, allowing toxins and bacteria to escape into your system. This phenomenon, known as “leaky gut,” triggers your immune system to react, leading to chronic inflammation.
This inflammation doesn’t just stay localized in your gut. It can spread throughout your body, affecting various organs and tissues, including your ovaries. Chronic inflammation can exacerbate the symptoms of PCOS by disrupting your hormonal balance. For example, inflammation can impair insulin signaling, leading to insulin resistance – a hallmark of PCOS.
Moreover, hyperandrogenism, or elevated levels of male hormones, is closely linked to gut health. Research indicates that your gut microbiota can influence sex hormone production. In those with PCOS, an imbalanced gut microbiota may contribute to increased testosterone levels, worsening symptoms like excess hair growth, acne, and menstrual irregularities.
Addressing inflammation through gut health can be a powerful strategy. By focusing on a diet rich in anti-inflammatory foods, you can help restore balance to your gut microbiota. Probiotics, prebiotics, and other dietary supplements may also play a vital role in reducing inflammation and supporting a healthier hormonal balance.
The Role of Inflammation in PCOS and Gut Health
Chronic inflammation is a known factor in the development of PCOS. Chronic inflammation is a hallmark of PCOS, often linked to an imbalance in gut microbiota. When your gut bacteria are out of balance, it can lead to increased intestinal permeability, commonly known as “leaky gut.” This condition allows toxins and partially digested food particles to enter the bloodstream, triggering an immune response and chronic inflammation.
This persistent inflammation can exacerbate insulin resistance, a common feature in PCOS. Insulin resistance leads to elevated blood sugar levels, which in turn can cause the body to produce more insulin. High insulin levels stimulate the ovaries to produce more androgens, contributing to symptoms such as irregular menstrual cycles, acne, and hirsutism.
Moreover, chronic inflammation influences ovarian function and insulin sensitivity through various biochemical pathways. For instance, certain inflammatory markers like IL-22 have been shown to affect ovarian granulosa cells, which are crucial for hormone production and ovarian health. Inflammatory cytokines can also disrupt the normal functioning of the ovaries, potentially worsening PCOS symptoms.
It’s also worth noting that Vitamin D deficiency, commonly observed in PCOS patients, can further exacerbate inflammation. Vitamin D has anti-inflammatory properties, and its lack can lead to an increase in inflammatory responses, thereby worsening both gut health and PCOS symptoms. It is also known that Women with PCOS often have altered gut microbiota compared to those without PCOS.
Given this intricate relationship, addressing inflammation by improving gut health can be a promising approach to managing PCOS. Incorporating anti-inflammatory foods, probiotics, and dietary changes can help maintain a balanced gut microbiota, reduce intestinal permeability, and ultimately mitigate the inflammatory processes that contribute to PCOS.
Recognizing the Signs of Poor Gut Health
Recognizing the signs of poor gut health is crucial in managing PCOS effectively. You might wonder what symptoms to look out for. Here’s a quick guide to help you identify potential gut issues:
- Digestive discomfort: Frequent bloating, gas, diarrhea, or constipation could indicate an imbalance in your gut microbiota.
- Food intolerances: If you notice increased sensitivity to certain foods, it might be linked to gut health issues.
- Fatigue: Chronic tiredness can be a sign that your gut is not absorbing nutrients properly.
- Skin conditions: Issues like eczema or acne can be linked to gut health, as inflammation in the gut often manifests on the skin.
- Mood changes: An unbalanced gut microbiota can lead to abnormal hormone changes, potentially contributing to anxiety and mood swings.
- Unintentional weight changes: Both weight gain and loss without any obvious reason can indicate a gut health problem.
It’s important to be attentive to such signs because they can be early indicators of more significant issues. If you experience any of these symptoms consistently, it might be time to take a closer look at your gut health, especially if you have PCOS.
Dietary Changes to Boost Gut Health for PCOS
Making the right dietary choices can significantly influence your gut health and, by extension, help manage symptoms of PCOS. Let’s delve into some practical and effective changes you can implement.

1. Incorporate Fiber-Rich Foods
Fiber acts as fuel for the beneficial bacteria in your gut. Eating a diet rich in fruits, vegetables, whole grains, and legumes can support these bacteria, which in turn helps regulate hormones and reduce inflammation. Aim to include at least 25-30 grams of fiber daily.
2. Add Fermented Foods

Fermented foods such as yogurt, kefir, sauerkraut, kimchi, and kombucha are brimming with probiotics. Regularly consuming these foods can help restore and maintain a healthy gut microbiota, crucial for managing PCOS symptoms. Probiotics, like bifidobacterium lactis V9, in particular, have shown promising results in improving gut health for women with PCOS.
3. Focus on Prebiotics
Prebiotics are non-digestible food ingredients that promote the growth of beneficial bacteria. Foods like garlic, onions, bananas, asparagus, and oats are excellent prebiotic sources. Integrating these into your diet can help nurture a healthy gut environment. Probiotics and prebiotics can positively influence gut microbiota.
4. Opt for Healthy Fats
Healthy fats, particularly those from omega-3 fatty acids, can reduce inflammation and support overall gut health. Include sources such as fatty fish (salmon, mackerel), flaxseeds, chia seeds, and walnuts in your meals to reap their benefits.
5. Minimize Processed Foods and Sugars
Highly processed foods and sugary snacks can promote harmful bacteria growth and contribute to gut dysbiosis. Steering clear of these foods can help maintain a balanced gut microbiome, which is crucial for managing PCOS effectively.
By making these dietary adjustments, you can create a supportive environment for your gut health, potentially alleviating some of the hormonal and metabolic challenges associated with PCOS. Remember, small, consistent changes can lead to significant improvements over time.
Supplements That Support Gut Health in PCOS
Supplements can play a significant role in supporting gut health, particularly for women managing PCOS. Integrating the right supplements into your routine can help rebalance your gut microbiota, leading to improved overall health.

Probiotics
One of the most well-researched supplements for gut health is probiotics. Strains like Bifidobacterium lactis V9 have shown promise in improving gut health in women with PCOS. Probiotics can help restore the natural balance of gut bacteria, which in turn may enhance metabolic and reproductive functions. One of our favorites is Megaspore biotic – which you can find inside our supplement store right here.
Prebiotics
Prebiotics are another cornerstone of gut health. These are non-digestible fibers that fuel the growth of beneficial bacteria in your gut. Incorporating prebiotic supplements can create a more favorable environment for your gut microbiota, helping to improve hormonal balance and reduce inflammation, both crucial for managing PCOS.
Synbiotics
Combining probiotics and prebiotics, synbiotics offer dual benefits. By taking these supplements, you provide your gut with beneficial bacteria while ensuring they have the nutrients they need to thrive. This synergistic approach can be particularly effective for restoring gut microbiota diversity and improving PCOS symptoms.
Vitamin D
Emerging research suggests that Vitamin D might influence the occurrence of PCOS by affecting the composition of gut microbiota. Vitamin D supplementation could improve gut health and potentially alleviate some symptoms of PCOS by enhancing the microbiota balance. *It’s important to test vitamin D levels before supplementing, as you can go *too high* with this as well.
Getting Support with Your Gut Health and PCOS
If you’re looking for more support with managing your PCOS, improving your gut health, and preparing your body for a healthy pregnancy, reach out to our team of highly trained functional fertility nutritionists.
We utilize functional lab testing such as the GI MAP, to help uncover the root cause of your fertility struggles. We’ve worked with hundreds of women in our practice, and are here to support you!

The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook
