Resources
Style
Planning
View All
THE blog
Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Did you know that your gut health could impact more than just digestion? From immunity to mental clarity, a healthy gut plays a pivotal role in overall well-being—and even fertility. Emerging research suggests that a balanced gut microbiome influences hormone regulation, immune function, and inflammation, all of which are crucial for reproductive health. Whether you’re looking to optimize fertility or improve general health, supporting your gut can be a game-changer for both your body and mind.
The Basic Functions of the Gut
Before diving into the more intricate details of gut health, it’s essential to understand the basic functions of the gut and why it plays such a crucial role in your overall health.
1. Digestion
The gut is responsible for breaking down the food we eat, allowing nutrients to be absorbed into the bloodstream. This process starts in the mouth and continues through the stomach and small intestine. Enzymes and acids help break down food into smaller molecules for absorption.
2. Nutrient Absorption
Once food is broken down, the small intestine absorbs essential nutrients—like vitamins, minerals, and amino acids—into the bloodstream. These nutrients are then transported throughout the body to fuel our cells and organs.
3. Immune Function
A large portion of the body’s immune system resides in the gut. It acts as a barrier to harmful pathogens, such as bacteria and viruses. A healthy gut microbiome— the community of beneficial bacteria—supports immune function and helps protect the body from infections and inflammation.
4. Detoxification
The gut plays a vital role in detoxifying the body by processing and eliminating waste. The liver, bile, and gut work together to filter out toxins, which are then excreted through the stool. This process helps maintain a clean internal environment.
5. Hormone Regulation
The gut is involved in hormone production and regulation. It helps control hormones related to digestion, hunger, and metabolism. Additionally, the gut microbiome can influence hormonal balance, which is vital for reproductive health.
6. Gut-Brain Connection
The gut and brain communicate through the gut-brain axis, a direct link between the two. This connection influences mood, mental clarity, and stress levels. Research suggests that an imbalance in the gut microbiome can impact mental health conditions like anxiety and depression.
By understanding these basic functions, we can see why maintaining a healthy gut is essential for overall well-being and fertility. Now, let’s dive deeper into how to support these functions for optimal health.
Understanding Gut Permeability and Leaky Gut
Leaky gut occurs when the intestinal barrier becomes compromised, allowing undigested food particles, toxins, and microbes to enter the bloodstream. This process can trigger systemic inflammation and is implicated in conditions like autoimmune diseases, irritable bowel syndrome (IBS), and even neuroinflammation. The protein zonulin regulates tight junctions in the gut lining, and its overproduction is associated with increased gut permeability.
Dietary choices, stress, and environmental toxins all influence this delicate balance.
The Role of Diet in Gut Health
Diet plays a crucial role in shaping gut microbiota and maintaining a strong intestinal barrier. Research suggests that:
- High-fiber foods (e.g., fruits, vegetables, whole grains) support beneficial bacteria and help regulate gut permeability.
- Healthy fats, such as omega-3s, promote anti-inflammatory gut conditions, whereas excessive saturated fat intake can negatively impact gut flora.
- Akkermansia muciniphila, a beneficial bacterium, is linked to improved gut barrier function, reduced inflammation, and better metabolic health.
- Bovine colostrum supplementation has been shown to decrease intestinal permeability and lower zonulin levels, particularly in athletes.
Small Intestinal Bacterial Overgrowth (SIBO) and Gut Dysfunction
SIBO occurs when there’s an overgrowth of bacteria in the small intestine. This can lead to bloating, malabsorption, and digestive discomfort. It’s often associated with IBS, celiac disease, and metabolic syndrome.
Managing SIBO:
- Get proper testing to identify SIBO.
- Modify your diet, focusing on low FODMAP foods.
- Consider probiotics to restore balance.
- Work with a healthcare provider to determine if antibiotics are necessary.
Gut Health and Systemic Wellness
Emerging research highlights the gut-brain connection, linking gut health to cognitive function, mood regulation, and neurological diseases like Alzheimer’s. The gut microbiome also plays a role in cardiovascular health, obesity, and diabetes. Fecal microbiota transplants (FMT) have even been explored as potential treatments for age-related cognitive decline and metabolic disorders.
Gut Health and Fertility
Emerging research suggests that gut health plays a crucial role in reproductive health. The gut microbiome influences hormone regulation, immune function, and inflammation, all of which impact fertility outcomes. Dysbiosis, or an imbalance of gut bacteria, has been linked to conditions like polycystic ovary syndrome (PCOS), endometriosis, and unexplained infertility.
- Hormonal Balance: The gut microbiome helps regulate estrogen levels through the estrobolome, a collection of bacteria involved in estrogen metabolism. An imbalance can lead to estrogen dominance, which is associated with infertility and conditions like PCOS.
- Inflammation and Immune Function: Chronic inflammation, often driven by poor gut health, has been implicated in endometriosis and implantation failure. A healthy gut barrier helps regulate immune responses and supports a favorable reproductive environment.
- Microbiome and Pregnancy Outcomes: Research suggests that a balanced gut microbiome contributes to healthy pregnancy outcomes, reducing the risk of gestational diabetes, preeclampsia, and preterm birth.
Supporting Digestion
Efficient digestion breaks down food properly, allowing for optimal nutrient absorption and minimizing digestive distress.
Ways to enhance digestion include:
- Incorporating bitter foods: Foods like arugula, artichoke, bitter melon, dandelion greens, Brussels sprouts, coffee, and grapefruit stimulate stomach acid and bile production.
- Using digestive aids: Digestive enzymes, HCl supplements, apple cider vinegar, or digestive bitters may be beneficial.
- Relaxing at meals: Stress can negatively impact digestion, so mindful eating practices are essential.
- Consuming adequate minerals: Sodium (from sea salt) and zinc (from oysters and red meat) support stomach acid production.
Supporting Healthy Bile Flow
Bile is critical for fat digestion and detoxification. Signs of inadequate bile include bloating, floating stools, nausea after eating fats, and vitamin deficiencies. To support bile production:
- Consume fiber-rich foods: Legumes, beans, and avocados help bind to excess bile.
- Eat bitter foods: These naturally promote bile flow.
- Use cholagogue herbs: Globe artichoke, dandelion, burdock, and Oregon grape enhance bile movement.
- Ensure adequate taurine intake: Meat, fish, shellfish, and eggs aid in bile salt production.
Supporting Beneficial Bacteria
A balanced gut microbiome is essential for digestion, immunity, and gut barrier integrity. To nurture beneficial bacteria:
- Prioritize digestion first: Ensuring proper food breakdown is key before increasing fiber intake.
- Incorporate prebiotic foods: Apples, asparagus, garlic, onions, oats, and legumes serve as fuel for gut bacteria.
- Limit excessive alcohol intake: Alcohol can cause dysbiosis and inflammation.
Supporting Liver Detoxification
The liver plays a crucial role in gut health through bile production and detox processes. To support liver function:
- Include Phase 1 detox foods: Magnesium (leafy greens, avocado), B vitamins (liver, eggs, seafood), vitamin C (citrus, bell peppers), and zinc (oysters, beef).
- Incorporate Phase 2 detox foods: Glycine (bone broth), glutamine (beef, spinach), cysteine (broccoli, eggs), and taurine (meat, fish).
Strengthening the Gut Lining
A strong intestinal barrier prevents harmful substances from entering the bloodstream. Factors that contribute to a leaky gut include stress, poor digestion, processed foods, overuse of medications, and imbalanced gut bacteria. To support gut integrity:
- Limit inflammatory foods: Avoid heavily processed and inflammatory oils.
- Boost beneficial fibers: Prebiotic and resistant starch-rich foods enhance gut lining health.
- Consume gut-supportive nutrients: Glutamine (cabbage, fish), zinc (beef, crab), and colostrum aid in healing the gut lining.
- Use gut-healing herbs: Marshmallow root, slippery elm, aloe vera, and licorice can be beneficial.
Strengthening the Immune System
A well-functioning immune system relies on strong digestion and a balanced gut microbiome. Factors that deplete immunity include poor digestion, chronic stress, hormonal imbalances, and long-term medication use. To support immune health:
- Improve digestion and gut microbiome health
- Incorporate immune-boosting foods: Colostrum, mushrooms (reishi, shiitake), and vitamin C-rich foods (citrus, mango, papaya) support immune function.
- Use supportive herbs: Andrographis, elderberry, echinacea, and astragalus help strengthen immunity.
Prebiotics & Resistant Starch
Prebiotics are fibers that feed beneficial bacteria and help produce short-chain fatty acids, which support gut integrity and immunity.
- Prebiotic foods: Apples, asparagus, garlic, onions, oats, and legumes.
- Resistant starch sources: Cooked and cooled potatoes, green bananas, and legumes.
By focusing on these key areas, you can create a solid foundation for optimal gut health and overall well-being. Making small, sustainable changes to your diet and lifestyle can have lasting positive effects on digestion, immunity, and energy levels.
Conclusion
Maintaining gut health is essential for overall well-being, from digestion and immunity to mental clarity and chronic disease prevention. By making mindful dietary and lifestyle choices, you can support a resilient gut microbiome and improve long-term health outcomes. The science is clear: a healthy gut is a foundation for a thriving body and mind.

Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996528/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8305009/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6313445/
- https://pubmed.ncbi.nlm.nih.gov/38790992/
- https://pubmed.ncbi.nlm.nih.gov/32023228/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8058106/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8674859/
- https://pubmed.ncbi.nlm.nih.gov/25290618/
- https://pubmed.ncbi.nlm.nih.gov/35874661/
- https://pubmed.ncbi.nlm.nih.gov/34623232/
- https://www.imrpress.com/journal/FBL/26/5/10.52586/4921/htm
- https://www.nia.nih.gov/news/beyond-brain-gut-microbiome-and-alzheimers-disease
- https://pubmed.ncbi.nlm.nih.gov/34054740/
- https://pubmed.ncbi.nlm.nih.gov/28397754/
- https://pubmed.ncbi.nlm.nih.gov/35745242/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7971312/
- https://pubmed.ncbi.nlm.nih.gov/28778332/
Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Thinking about starting a family? Have you ever wondered what you can do before trying to conceive to boost your chances of a healthy pregnancy? Your fertility journey starts long before a positive pregnancy test. Preparing for pregnancy isn’t just about tracking ovulation and taking prenatal vitamins—it’s about optimizing your entire body for conception and a healthy pregnancy. Scientific research increasingly shows that preconception health plays a crucial role in reproductive success and fetal development. Here are five key areas you can’t afford to skip when getting ready to grow your family.
1. Support Your Gut Health
Your digestive system isn’t just about breaking down food—it’s a complex ecosystem that plays a central role in your overall health, including fertility. A healthy gut microbiome, which refers to the trillions of bacteria, fungi, and other microbes living in your digestive system, influences numerous physiological functions, from hormone regulation to immune function and even mood.
The connection between gut health and fertility is emerging as an important area of study. Research increasingly shows that an imbalanced gut microbiome, also known as dysbiosis, can have a significant impact on fertility. When the gut microbiome is out of balance, it can lead to inflammation, hormonal imbalances, and poor nutrient absorption—all of which can affect your ability to conceive.
The Gut Microbiome and Hormone Regulation
A healthy gut microbiome is essential for maintaining hormonal balance, which is crucial for fertility. The gut bacteria help metabolize estrogens, which are important for regulating the menstrual cycle and maintaining a healthy ovulation pattern. Dysbiosis has been linked to estrogen dominance, which can interfere with ovulation and lead to conditions like polycystic ovary syndrome (PCOS), a common cause of infertility.
The microbiome also plays a key role in detoxifying estrogen and other hormones, helping to prevent an overload of hormones that can disrupt your reproductive system. When the gut is not functioning optimally, it can lead to a build-up of excess estrogen in the body, a condition known as estrogen dominance, which can impact fertility and cause other reproductive health problems.
Gut Health and Immune Function
In addition to influencing hormones, the gut microbiome also affects your immune system. Around 70% of the body’s immune cells reside in the gut, and the microbiome plays a vital role in maintaining immune balance. A healthy immune system is essential for fertility because an overactive or dysfunctional immune response can interfere with embryo implantation and fetal development. Chronic inflammation in the gut can trigger an autoimmune response, leading to complications in fertility and pregnancy.
Studies have shown that women with autoimmune diseases, such as endometriosis or thyroid disorders, often have gut dysbiosis, which could be contributing to their fertility struggles. This means addressing gut health may also help reduce inflammation and autoimmune responses, creating a more favorable environment for conception and pregnancy.
The Role of Diet in Gut Health
Your diet plays a crucial role in shaping your gut microbiome. The foods you eat provide fuel for your gut bacteria, and by choosing nutrient-dense, whole foods, you can encourage the growth of beneficial microbes that support both gut and reproductive health.
To promote a healthy gut microbiome and support fertility:
- Eat fiber-rich foods: A diet high in fruits, vegetables, whole grains, and legumes provides the necessary fiber to feed beneficial gut bacteria. Fiber acts as a prebiotic, helping to nourish the good bacteria in your gut that help regulate hormones and immune function.
- Include fermented foods: Fermented foods such as yogurt, kefir, sauerkraut, kimchi, and kombucha contain probiotics, which are live beneficial bacteria that help restore balance to the gut microbiome. These foods support the growth of healthy bacteria, improve digestion, and reduce inflammation, all of which are essential for fertility.
- Limit processed foods and sugar: Processed foods, refined sugars, and artificial sweeteners can encourage the growth of harmful bacteria in the gut, leading to an imbalance in the microbiome. This imbalance can contribute to inflammation and poor immune function, both of which can hinder fertility.
Addressing Gut Dysbiosis for Fertility
If you suspect that gut dysbiosis may be affecting your fertility, it’s important to work with a healthcare professional, such as a dietitian or functional medicine practitioner, to assess and address the issue. Common signs of dysbiosis include digestive symptoms like bloating, gas, constipation, diarrhea, and food intolerances. A professional can help guide you through dietary changes and supplements, such as probiotics or antimicrobial herbs, to support gut health and restore balance to your microbiome. Some studies have suggested that the use of probiotics and other gut-healing supplements may improve fertility outcomes, particularly in women with PCOS and other reproductive health conditions.
By supporting your gut health, you’re not just promoting better digestion and immune function—you’re creating a favorable environment for fertility.
Learn more about gut health and fertility
2. Balance Blood Sugar
Maintaining balanced blood sugar is crucial for overall health, especially when preparing for pregnancy. Blood sugar imbalances, such as insulin resistance and high blood glucose levels, can interfere with ovulation, hormone production, and overall fertility. In fact, managing blood sugar levels can be one of the most effective ways to optimize reproductive health and enhance fertility. Here’s why blood sugar balance matters and how you can achieve it.
How Blood Sugar Affects Fertility
Blood sugar imbalances, particularly insulin resistance, can have a significant impact on fertility. Insulin is a hormone that regulates blood sugar levels, and when the body becomes resistant to insulin, it needs to produce more of it to maintain normal blood glucose levels. High insulin levels can disrupt the balance of other hormones that regulate reproductive function, such as estrogen, progesterone, and testosterone. In addition to disrupting ovulation, high insulin levels can also impact the quality of the eggs and the ability to support a pregnancy.
The Link Between Blood Sugar and Hormone Imbalance
The relationship between blood sugar and hormone balance is intricate. Insulin not only regulates glucose levels but also interacts with other hormones like cortisol, leptin, and thyroid hormones, all of which play essential roles in fertility. High insulin levels can lead to an imbalance in these hormones, affecting reproductive function.
For example:
- Cortisol: Chronic stress and high blood sugar levels can elevate cortisol, a stress hormone that disrupts hormone production and reduces fertility. High cortisol levels can lead to irregular menstrual cycles and impair ovulation.
- Leptin: Leptin is a hormone produced by fat cells that helps regulate appetite, metabolism, and reproductive function. Imbalances in leptin levels, often seen in individuals with insulin resistance, can interfere with ovulation and menstrual regularity.
- Insulin resistance can also disrupt thyroid function, which is crucial for fertility. Studies have shown that insulin resistance can lead to hypothyroidism (low thyroid function), which can cause menstrual irregularities, poor egg quality, and difficulty getting pregnant.
How to Balance Blood Sugar for Fertility
Achieving and maintaining stable blood sugar levels is a key factor in preparing for pregnancy. Here are some practical steps you can take to balance your blood sugar:
Prioritize Protein, Fiber, and Healthy Fats
Including a balance of protein, fiber, and healthy fats at each meal can help stabilize blood sugar levels. These nutrients slow the absorption of glucose into the bloodstream, preventing spikes in blood sugar. Focus on lean protein sources (such as chicken, fish, tofu, and legumes), fiber-rich vegetables and whole grains, and healthy fats (like avocado, nuts, and olive oil).
Minimize Refined Carbs and Sugar
Refined carbohydrates (such as white bread, pasta, and baked goods) and sugary foods cause rapid spikes in blood sugar, followed by crashes that can lead to insulin resistance over time. Instead, opt for whole grains, vegetables, and fruits that release sugar more slowly into the bloodstream, providing a steady supply of energy.
Regular Physical Activity
Exercise, especially strength training, helps improve insulin sensitivity, meaning your body uses insulin more effectively to regulate blood sugar. Studies have shown that regular physical activity, including moderate aerobic exercise and strength training, can improve metabolic function and support healthy hormone levels, thereby enhancing fertility.
Manage Stress
Chronic stress can elevate cortisol levels, which in turn disrupt blood sugar regulation and fertility. Incorporating stress-management techniques such as deep breathing, meditation, yoga, or spending time in nature can help lower cortisol levels and improve overall hormonal balance.
Consider Supplements
Certain nutrients, such as magnesium, chromium, and omega-3 fatty acids, may help support healthy blood sugar metabolism. Magnesium, in particular, is important for insulin function, and research has shown that adequate magnesium levels are associated with better fertility outcomes.
Managing blood sugar not only supports fertility but also helps set the stage for a healthy pregnancy by lowering the risk of complications like gestational diabetes.
Explore blood sugar management strategies
3. Detox Your Environment
Endocrine-disrupting chemicals (EDCs), found in plastics, pesticides, pollution, and personal care products, can interfere with hormone balance and reproduction. Research shows that exposure to EDCs—such as BPA, phthalates, and pesticides—can affect fertility by disrupting hormone production and ovarian function.
The 4 P’s to Avoid:
- Plastics: Opt for glass or stainless steel for food storage and drink containers to reduce exposure to BPA and phthalates, which have been linked to reduced ovarian reserve and lower sperm quality.
- Pesticides: Choose organic produce when possible and thoroughly wash fruits and vegetables. Pesticides can disrupt estrogen and progesterone levels, hindering reproductive success.
- Pollution: Use air purifiers and avoid high-traffic areas to minimize exposure to air pollution, which can lower fertility rates and increase miscarriage risk.
- Personal Care Products: Swap conventional beauty, skincare, and cleaning products for non-toxic alternatives. Parabens and synthetic fragrances found in many products are linked to hormone disruption and reduced fertility.
Reducing your exposure to these toxins can help protect your hormones and reproductive health.
Learn more about reducing toxic exposure
4. Optimize Sleep & Manage Stress
Poor sleep and chronic stress can raise cortisol levels, negatively impacting reproductive hormones and fertility. Disrupted sleep patterns—such as waking up between 1-3 AM—may indicate liver detoxification issues, while difficulty staying asleep or waking up feeling unrested often correlates with low progesterone levels. Stress can lead to irregular cycles, making conception more difficult.
Studies show that sleep disturbances and high stress levels can disrupt menstrual cycle regularity, reduce ovarian function, and even affect early pregnancy outcomes.
To improve sleep and reduce stress:
- Stick to a consistent sleep schedule, even on weekends.
- Avoid blue light exposure from screens at least an hour before bed.
- Create a calming nighttime routine—try magnesium, herbal teas, or journaling.
- Get sunlight exposure in the morning to regulate circadian rhythms.
Stress-reducing activities like meditation, breathwork, and yoga can support your fertility by lowering cortisol levels.
5. Assess Your Partner’s Health
Fertility is a team effort! Around 40% of infertility cases involve male factors, and sperm health plays a major role in conception. Changes in diet, lifestyle, and environmental exposure can improve sperm quality, motility, and count. Since sperm takes about 74 days to regenerate, it starts by making changes at least three months before conception.
To support male fertility:
- Nutrient-dense foods rich in zinc, selenium, omega-3 fatty acids, and antioxidants are essential for sperm health. Zinc and selenium, in particular, play critical roles in sperm formation and motility.
- Limit alcohol and cannabis use, as both can reduce sperm concentration and motility.
- Avoid excessive heat—hot tubs, saunas, and even laptops on laps can lower sperm count. The testes require a cooler temperature for optimal sperm production.
- Reduce stress—high cortisol levels can lower testosterone and sperm quality.
The father’s lifestyle before conception can influence the baby’s long-term health through epigenetic changes, which may affect gene expression in both parents.
Learn more about understanding cortisol
The Bottom Line
Prepping for pregnancy isn’t just about waiting for a positive test—it’s about creating the healthiest possible environment for conception and beyond. By addressing gut health, blood sugar balance, environmental toxins, sleep, and both partners’ health, you’re laying the groundwork for a smoother fertility journey. Small, intentional choices today can make a big difference tomorrow. Take control of your health today!
Start your journey to optimal fertility

Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC9603966
https://pmc.ncbi.nlm.nih.gov/articles/PMC5052775
https://www.sciencedirect.com/science/article/pii/S245196502030079X
https://www.cdc.gov/genomics-and-health/epigenetics/index.html
https://www.hopkinsmedicine.org/health/wellness-and-prevention/planning-a-pregnancy
https://pmc.ncbi.nlm.nih.gov/articles/PMC6075697
https://pmc.ncbi.nlm.nih.gov/articles/PMC4145858

By: Anabelle Harari Clebaner MS, RDN
Diet impacts everything
Want to boost fertility? 🌟 Start with what’s on your plate. Yep, your diet can make a HUGE difference.
When it comes to fertility, adequate nutrition plays a pivotal role. The right nutrients can significantly influence your reproductive health, improving your chances of conception and a healthy pregnancy.
As a fertility dietitian, I know firsthand just how much nutrition makes an impact on your reproductive health, after working with hundreds of women in my private practice, Wellspring Nutrition.
Think of it this way – you have three opportunities every single day to make a healthy choice that nourishes your body for fertility and pregnancy.
So let’s get right into it – here are 5 foods you can start to incorporate or increase in your diet to start to see positive changes in your fertility.
Leafy greens: The superstars 🌿
Spinach, kale, and their leafy friends are packed with folate, iron, and antioxidants.
Folate is essential for: DNA synthesis and repair, embryonic development, and preventing neural tube defects.
Folic acid is crucial for both men and women. For women, it helps create a healthy environment for egg fertilization and early embryonic growth. For men, it supports healthy sperm production.
Iron is essential for: Hemoglobin production and oxygen transport.
Adequate iron levels prevent anemia, which can affect ovulation and overall energy levels, making your body more conducive to conception.
These nutrients are your fertility BFFs. Add them to salads, smoothies, or soups. Easy peasy!
Fatty fish: Omega-3 magic 🐟
We can’t have a conversation about Omega-3 fats without also talking about Omega-6 fats.
Both Omega-3 and Omega-6 fatty acids are essential polyunsaturated fats, meaning your body cannot produce them, and they must be obtained through your diet. Despite being in the same family of fats, they have different roles and effects on the body.
The three most important types are:
– **EPA (Eicosapentaenoic Acid)**: Found in fatty fish such as salmon, mackerel, and sardines. – **DHA (Docosahexaenoic Acid)**: Also found in fatty fish and is a crucial component of brain and eye health.
– **ALA (Alpha-Linolenic Acid)**: Found in plant sources like flaxseeds, chia seeds, and walnuts.
ALA can be converted to EPA and DHA in the body, but this process is relatively inefficient.

Health Benefits
**Anti-Inflammatory**: Omega-3s help reduce inflammation in the body, which can lower the risk of chronic diseases such as heart disease and arthritis. – **Cardiovascular Health**: They are known for their heart-protective effects, reducing blood pressure, and improving cholesterol levels. – **Mental Health**: Omega-3s play a crucial role in brain health and have been linked to reduced symptoms of depression and anxiety. – **Fertility**: As mentioned earlier, they improve egg quality, regulate ovulation, and reduce the risk of endometriosis.
Omega-6 Fatty Acids
Types
The most common type is: – **LA (Linoleic Acid)**: Found in vegetable oils like sunflower, soybean, and corn oil. – **AA (Arachidonic Acid)**: Found in meat and eggs; it is derived from LA. – **GLA (Gamma-Linolenic Acid)**: Found in evening primrose oil and blackcurrant seed oil; it’s a less common omega-6.
Health Benefits
**Pro-Inflammatory and Anti-Inflammatory**: Omega-6 fats can produce both pro-inflammatory and anti-inflammatory compounds. The body’s balance of omega-6 to omega-3 determines the effect. – **Skin Health**: Omega-6 fatty acids can help support skin barrier function and hydration. – **Growth and Development**: Essential for normal growth and brain function, particularly in children.
Key Differences
**Balance and Ratio** – **Ideal Ratio**: Historically, humans consumed Omega-3 and Omega-6 fats in a balanced ratio of about 1:1 to 1:4. However, modern diets tend to have a ratio closer to 1:20 or 1:30, significantly skewed towards Omega-6, leading to an imbalance.
**Health Impact**: An imbalanced ratio (high in Omega-6 and low in Omega-3) can promote inflammation and contribute to chronic diseases. Ensuring an adequate intake of Omega-3s while reducing excessive Omega-6s can optimize health.
Sources
**Omega-3s**: Primarily found in fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, walnuts, and algae.
**Omega-6s**: Found mostly in vegetable oils, nuts, seeds, and processed foods. They are more prevalent in the typical Western diet.
While both Omega-3 and Omega-6 fatty acids are essential for health, maintaining a proper balance between them is crucial. Increasing your Omega-3 intake and being mindful of Omega-6 consumption can help in achieving better overall health and reducing the risk of chronic diseases.
Omega-3 Fatty Acids are Essential for: Reducing inflammation, hormone production, and cell membrane function.
Omega-3 fatty acids are known to improve egg quality, regulate ovulation, and reduce the risk of endometriosis. For men, they improve sperm quality and mobility.
So where do you find Omega-3 fatty acids? Salmon, mackerel, and sardines are where it’s at. These fatty fish are fertility wonders. Grill ’em, bake ’em, or toss ’em in a salad. Your future self will thank you.
Nuts and seeds: Tiny powerhouses 🥜
Pumpkin seeds, walnuts, and almonds are considered tiny powerhouses because they are bursting with zinc and selenium. When it comes to fertility, both zinc and selenium play critical roles in ensuring optimal reproductive health. These essential trace minerals are involved in numerous bodily functions, specifically those related to reproductive health for both men and women.

Zinc
Zinc is vital for:
- Hormone Regulation: Zinc helps in regulating hormone levels, particularly testosterone in men and estrogen and progesterone in women. Balanced hormone levels are crucial for a healthy reproductive system.
- Sperm Production and Quality: In men, zinc is essential for spermatogenesis, the process of sperm production. It also enhances sperm motility and morphology, crucial factors for successful fertilization.
- Ovulation: For women, zinc supports the maturation of eggs and ensures regular ovulation, which is essential for conception.
- DNA Synthesis: Zinc is involved in DNA synthesis and cell division, processes that are fundamental during the early stages of fetal development once conception occurs.
Selenium
Selenium contributes to fertility by:
- Antioxidant Support: Selenium acts as a powerful antioxidant, protecting reproductive cells from oxidative stress, which can damage sperm and eggs.
- Thyroid Function: Proper thyroid function, supported by selenium, is crucial for fertility. The thyroid gland regulates many metabolic processes, including those that affect reproductive health.
- Sperm Quality: In men, selenium is essential for the formation and motility of sperm. It helps in maintaining the integrity and function of sperm cells.
- Development: Selenium plays a role in the early stages of embryo development by ensuring proper DNA synthesis and protecting against cellular damage.
Snack on them, throw them in your oatmeal, or mix them in a trail mix – there’s no way to go wrong here! And if you want to learn more about seed cycling, check out this blog right here.
Berries: Antioxidant champs 🍓
Blueberries, strawberries, and raspberries are loaded with antioxidants. These little champs keep your reproductive system in top shape. Enjoy them fresh, frozen, or in a smoothie. Yum!
Antioxidants are compounds that help protect the body from oxidative stress, which is caused by an excess of free radicals—unstable molecules that can damage cells.
Free radicals are naturally produced during metabolism, but environmental factors like pollution, UV exposure, and poor diet can increase their levels.

Berries Images – Free Download on Freepik
Importance of Antioxidants for Fertility
1. **Protecting Reproductive Cells**: Antioxidants help neutralize free radicals, reducing oxidative stress on reproductive cells like sperm and eggs. This protection is crucial for maintaining the health and viability of these cells.
2. **Improving Egg Quality**: Oxidative stress can negatively affect egg quality, leading to issues like chromosomal abnormalities. Antioxidants can improve the quality and viability of eggs by reducing this stress.
3. **Enhancing Sperm Health**: In men, antioxidants play a vital role in protecting sperm from oxidative damage, which can affect sperm count, motility, and overall fertility.
4. **Supporting Hormonal Balance**: Certain antioxidants, like vitamin E and Coenzyme Q10, are involved in hormone production and regulation, which is essential for fertility.
5. **Reducing Inflammation**: Antioxidants like vitamin C, E, and selenium have anti-inflammatory properties, which can help reduce inflammation in the reproductive organs, supporting overall fertility.
Including a variety of antioxidant-rich foods like berries, nuts, seeds, leafy greens, and colorful vegetables can be beneficial for those looking to optimize their fertility.
Eggs: The complete package 🍳
Eggs—especially organic, free-range ones—are amazing. They’re packed with choline and protein, both super important for fertility. Scramble them, poach them, or make a frittata. So versatile!
Eggs are an excellent food for fertility, and one of the key reasons is their high content of choline, an essential nutrient that plays a significant role in reproductive health.

Eggs Pictures [HD] | Download Free Images on Unsplash
Choline and Fertility
1. **Cell Membrane Formation**: Choline is crucial for the formation and maintenance of cell membranes. This is particularly important during pregnancy, as it supports the development of the baby’s brain and nervous system. In the context of fertility, choline ensures the health and integrity of reproductive cells, such as eggs and sperm.
2. **Gene Expression**: Choline is involved in methylation, a process that regulates gene expression. Proper methylation is essential for DNA synthesis and repair, which is vital for healthy cell division and the development of a viable embryo.
3. **Reducing Neural Tube Defects**: Adequate choline intake during pregnancy is associated with a lower risk of neural tube defects in the developing baby. For those trying to conceive, ensuring sufficient choline intake can help prepare the body for a healthy pregnancy.
4. **Supporting Hormone Production**: Choline is a precursor to acetylcholine, a neurotransmitter that plays a role in muscle control and memory but also supports hormone production and regulation. Balanced hormone levels are crucial for ovulation and overall reproductive health.
Other Nutrients in Eggs
In addition to choline, eggs are packed with other nutrients that support fertility:
– **Protein**: Eggs are an excellent source of high-quality protein, essential for the growth and repair of tissues, including reproductive tissues.
– **Healthy Fats**: The healthy fats in eggs, including omega-3 fatty acids, support hormone production and reduce inflammation.
– **Vitamins and Minerals**: Eggs are rich in vitamins like B12, D, and A, as well as minerals like selenium and zinc, all of which play important roles in reproductive health.
Practical Tips
– **Whole Eggs**: Most of the choline in eggs is found in the yolk, so it’s important to consume whole eggs rather than just egg whites.
– **Balanced Diet**: Including eggs as part of a balanced diet can provide a variety of essential nutrients that collectively support fertility. Pairing eggs with other fertility-boosting foods like leafy greens, avocados, and whole grains can further enhance their benefits.
Incorporating eggs into your diet, especially for those looking to boost fertility, is a simple and effective way to ensure you’re getting enough choline and other vital nutrients.
Conclusion: Make it a habit
So, there you have it—the top 15 fertility-boosting foods – phew! That was a lot. Start adding these to your daily meals to reap all the benefits!
And if you’re looking for a super easy way to incorporate these foods, and so many others that are vital for fertility, check out my four-week fertility meal plan.
It was designed to take all of the nutrients important for fertility and translate it into delicious, healthy, and simple recipes to naturally nourish your fertility.
Whether you’re planning your next IUI cycle or are just getting started on your preconception journey, investing in your health is always worth it!
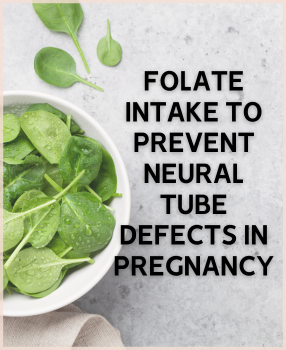
If you are currently pregnant, the journey of sustaining a whole other life in your body probably feels like an extraordinary experience but at the same time, a great deal of responsibility ( in a positive way of course! )
Although there are many aspects relating to the healthy growth and development of the fetus that are beyond our control, one of the main factors that we do have control over is our lifestyle choices- namely our diet.
There are a handful of nutrients that you do not want to be missing out on during your pregnancy to ensure the best possible health outcome for your baby. These include choline, iron, calcium, Vitamin D, iodine, and folate to name a few.
If you recently found out that you are pregnant or are planning on conceiving, you are in luck! Today, Wellspring Nutrition is specifically going to highlight the importance of folate, and how this nutrient can be a powerful ally for preventing a common type of birth defect- the neural tube defect.
What is a Neural Tube Defect?
Neural tube defect is a birth defect that affects the central nervous system of the baby. In a developing embryo, the neural tube is the precursor to their brain and the spinal cord. Neural tube defect occurs when the neural tube does not properly go through the closure process to complete its formation. The two common types of neural tube defect include:
- Spina bifida (swelling or protrusion of spinal cord or fluid in the back)
- Anencephaly (exclusion of a major segment of the brain)
What is folate?
Folate, otherwise known as vitamin B-9, is found in various foods. As they play an important role in the nucleic acid (DNA and RNA) production and amino acid (the building blocks of protein) metabolism, they are crucial to the functioning of cells.
Folic acid is its synthetic form- meaning folate that is found in dietary supplements and fortified foods.
Why folate is important
The need for folate significantly increases during pregnancy especially because the event of a neural tube defect is closely linked to maternal folate deficiency. Inadequate folate intake can lead to a high homocysteine level in the blood, which is considered to be a risk factor for neural tube defect. Homocysteine is an amino acid and as it is broken down by the vitamin B-complexes, having a high level of this usually indicates deficiency in vitamins.
According to a recent study, another risk factor for neural tube development is the lack of DNA repair function. Since folate is crucial to DNA synthesis, folate deficiency can lead to a loss in the integrity of DNA. Thus, the mechanism for DNA repair is going to be negatively impacted. Genome stability is an important aspect of neural development for the embryo, and adequate folate intake is necessary for a properly functioning DNA repair mechanism.
The timing of sufficient folate intake is important to consider. Neural tube formation of an embryo is completed around three to four weeks after conception. This means that anyone trying to conceive should ideally start incorporating folate in their diet as soon as possible, even if pregnancy is yet to be confirmed.
Even if you are reading this much further into your pregnancy, there are still reasons to consume an adequate amount of folate.
Other than lowering the risks of neural tube defects, research shows that sufficient folate intake during pregnancy is beneficial for the neurodevelopment of the child. There is a study that links prenatal folic acid supplementation to a lowering of the risk of Autism Spectrum Disorder (ASD), and advancements to the cognitive, motor and intellectual functions of the child.
What food should I eat for folate?
Although the general recommendation is about 400 micrograms a day, pregnant women are advised to consume about 600 micrograms of folate every day.
Here are some food items that are good sources of folate to help meet this target:
- Beef Liver
- Spinach
- Black-eyed peas
- Chickpeas
- Asparagus
- Brussel sprouts
- Romaine Lettuce
- Broccoli
- Eggs
As you can see, leafy greens, legumes, and liver are the best sources.
Moreover, it is important to note that folate tends to be sensitive to heat and oxygen. Especially for the leafy greens, it is advised to eat them fresh or have them lightly cooked. In a study that compared the folate retention for different food products, for spinach, boiling led to only 49 percent retention of folate. On the other hand, steaming proved to be the best way to preserve folate in vegetables. Another good news is that the same study found that grilling beef for an extended period of time did not result in much loss of folate as well.
Other than foods naturally present with folate, consuming grain products may be helpful as well. This is because starting in 1998, the U.S Food and Drug Administration (FDA) mandated a folate fortification of grain products such as bread, rice, cereal, flour, and pasta.
However, consumption of refined grain products should be limited during pregnancy to prevent significant spikes in your blood sugar levels.

Looking for more support?
Our fertility dietician Anabelle is available for one-on-one consultation and can help you address any of your concerns regarding fertility, pregnancy or hormonal imbalances like PCOS!
References
- “Chickpeas (garbanzo beans, bengal gram), mature seeds, cooked, boiled, without salt.” https://fdc.nal.usda.gov/fdc-app.html#/food-details/173757/nutrients
- “Embryology, Neural Tube.” https://www.ncbi.nlm.nih.gov/books/NBK542285/
- “Folate and Folic Acid on the Nutrition and Supplement Facts Labels.”https://www.fda.gov/food/new-nutrition-facts-label/folate-and-folic-acid-nutrition-and-supplement-facts-labels#:~:text=For%20folate%2C%20the%20DV%20is,consume%20500%20mcg%20DFE%20daily.
- Gao Y, Sheng C, Xie RH, Sun W, Asztalos E, Moddemann D, Zwaigenbaum L, Walker M, Wen SW. “New Perspective on Impact of Folic Acid Supplementation during Pregnancy on Neurodevelopment/Autism in the Offspring Children – A Systematic Review”PLoS One. 2016 Nov 22;11(11):e0165626. doi: 10.1371/journal.pone.0165626. eCollection 2016.PMID: 27875541 PMCID: PMC5119728 https://pubmed.ncbi.nlm.nih.gov/27875541/
- McKillop DJ, Pentieva K, Daly D, McPartlin JM, Hughes J, Strain JJ, Scott JM, McNulty H.“The effect of different cooking methods on folate retention in various foods that are amongst the major contributors to folate intake in the UK diet.” Br J Nutr. 2002 Dec;88(6):681-8. doi: 10.1079/BJN2002733. PMID: 12493090 https://pubmed.ncbi.nlm.nih.gov/12493090/
- “Pregnancy diet: Focus on these essential nutrients.”https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-nutrition/art-20045082
- Smith A, Colleen A, Spees C. “Wardlaw’s Contemporary Nutrition, 12th Edition.” McGraw Hill, 2022.
- Wang X, Yu J, Wang J.“Neural Tube Defects and Folate Deficiency: Is DNA Repair Defective?” Int J Mol Sci. 2023 Jan 22;24(3):2220. doi:10.3390/ijms24032220. PMID: 36768542 PMCID: PMC9916799 https://pubmed.ncbi.nlm.nih.gov/36768542/
Apple cider vinegarー the name surely gives it a cozy fall vibe doesn’t it?
Vinegar in general has demonstrated numerous health benefits but apple cider vinegar (ACV) , which is made from fermented apples, in particular has been gaining attention from many health experts in recent years (And no, ACV is not seasonalー thankfully it is around all year).
If you were curious as to what makes ACV beneficial to our health, you have come to the right place!
Blood sugar control:
Hyperglycemia, more commonly known as high blood sugar, affects countless people worldwide. This phenomenon is usually attributed to the lack of insulin in the body and is associated with both type 1 and type 2 diabetes. Insulin is a hormone that is secreted by the pancreas that controls what the body does with the energy obtained from food; it determines if it wants to use or store the blood sugar.
Research suggests that ACV may assist with glycemic control- that is our blood sugar levels.
Studies have shown that ACV consumption is associated with the overall reduction of blood glucose (sugar) levels.
Therefore, the consumption of ACV may serve as an ally for diabetes management as well as prevention.
Preventing cardiovascular diseases:
Now let’s talk cholesterol ー
Cholesterol travels throughout the bloodstream carried by “lipoprotein”, a type of protein.
There are two types of these lipoproteins: 1) LDL (low-density lipoprotein) cholesterol 2) HDL (high-density lipoprotein).
LDL is commonly referred to as the “bad” cholesterol while HDL is referred to as the “good” cholesterol. Since HDL, along with the liver, helps get rid of the cholesterol in the blood, higher HDL level can contribute to lowering the risk of cardiovascular diseases such as stroke, heart attack and peripheral artery disease.
ACV consumption was associated with higher levels of HDL for people who do not have diabetes.
Furthermore, studies have found that for those with type 2 diabetes, ACV consumption was linked to an improved lipid panel- a blood test that serves as a screening for cardiovascular diseases.
This blood test is based on cholesterol and triglycerides (a type of fat in our blood) levels. The buildup of these fats in the blood will lead to a hardening of the arteries and increase the risks of cardiovascular diseases. A decrease in both triglyceride and cholesterol levels in patients with type 2 diabetes was seen with the consumption of ACV.
Overall, this suggests a positive association between our heart health and ACV.
Antioxidative properties and other disease prevention:
ACV is said to have antioxidative and anti-inflammatory properties. There have been several studies that have linked such properties to the potential prevention and the remedy of kidney/urinary stones.
The kidney filters our blood, removes wastes from it and produces urine. It plays an important role in the body’s maintenance of the balance of fluid and minerals which is crucial for our physiological functioning.
Kidney stones are relatively common and may unfortunately lead to chronic kidney diseases. Although ACV should not be relied on as a sole treatment, its therapeutic effect says a lot about its defensive nature against oxidative stress and inflammation in our body.
Relatedly, ACV contains a phytochemical (compounds found in plants that can yield positive health effects) called flavonoid. Flavonoid have been found to have favorable effects on the following health complications:
- angina pectoris
- cervical lesions
- chronic venous insufficiency
- dermatopathy
- gastrointestinal diseases
- lymphocytic leukemia
- menopausal symptoms
- rhinitis
- traumatic cerebral infarction
Looking for more support?
If you would like to get more inspiration- whether it is about how to specifically incorporate ACV into your meals or anything related to concerns regarding PCOS and/or fertility struggles please feel free to check out our meal plans or any other services with our fertility dietician. We would love to provide guidance to your wellness journey!
References:
- “Familial Hyperlipidemia.” https://www.upmc.com/services/heart-vascular/conditions-treatments/hyperlipidemia#:~:text=Hyperlipidemia%20defines%20an%20elevated%20level,stroke%2C%20and%20peripheral%20artery%20disease.
- Gambaro G, Croppi E, Bushinsky D f, Jaeger P g, Cupisti Ad, Ticinesi A e, Mazzaferro S c, D’Addessi A b, Ferraro PM. “The Risk of Chronic Kidney Disease Associated with Urolithiasis and its Urological Treatments: A Review.” J Urol. 2017 Aug;198(2):268-273. doi: 10.1016/j.juro.2016.12.135. Epub 2017 Mar 10. PMID: 28286070
- Hadi A, Pourmasoumi M, Najafgholizadeh A, Clark CCT, Esmaillzadeh A. “The effect of apple cider vinegar on lipid profiles and glycemic parameters: a systematic review and meta-analysis of randomized clinical trials.” BMC Complement Med Ther 2021 Jun 29;21(1):179. doi: 10.1186/s12906-021-03351-w. PMID: 34187442 PMCID: PMC8243436
- “Hyperglycemia (High Blood Glucose)” https://diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hyperglycemia#:~:text=Hyperglycemia%20is%20the%20technical%20term,can’t%20use%20insulin%20properly.
- Kumar A, Nirmal P, Kumar M, Jose A, Tomer V, Oz E, Proestos C, Zeng M, Elobeid T, K S, Oz F. “Major Phytochemicals: Recent Advances in Health Benefits and Extraction Method.” Molecules. 2023 Jan; 28(2): 887. Published online 2023 Jan 16. Doi: 10.3390/molecules28020887 PMCID: PMC9862941 PMID: 36677944
- “LDL and HDL Cholesterol and Triglycerides.” https://www.cdc.gov/cholesterol/ldl_hdl.htm
- “Lipid Panel” https://my.clevelandclinic.org/health/diagnostics/17176-lipid-panel#:~:text=A%20lipid%20panel%20is%20a,a%20measurement%20of%20your%20triglycerides.
- “Phytochemicals.” https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals
- Singh AS, Singh A, Vellapandian C, Ramaswamy R, Thirumal M. “GC–MS based metabolite profiling, antioxidant and antiurolithiatic properties of apple cider vinegar.” Future Sci OA. 2023 Apr; 9(4): FSO855. doi: 10.2144/fsoa-2023-0035 PMCID: PMC10116371 PMID: 37090488
- “Your Kidneys & How They Work”https://www.niddk.nih.gov/health-information/kidney-disease/kidneys-how-they-work
Protein plays a vital role in supporting our health and wellness. Without proteins, our body would have trouble forming blood cells and other crucial structures, as well as regulating and maintaining its various functions.
A “high-protein diet” has become quite a buzzword in the health and the wellness field in recent years, especially in the realm of body-building or weight loss endeavors. As nutrition experts specializing in women’s health, we are going to specifically discuss the important relationship between sufficient protein intake and healthy pregnancy as well as potential impact for PCOS.
“I am currently pregnant- what should my protein intake look like?”
The current Recommended Dietary Allowance (RDA) for protein for adults is 0.8 grams of protein per kilogram of body weight. If a person weighs 154 pounds or 70 kilograms, 56 grams of protein would be the adequate daily intake.
However, for pregnant women, this recommendation is slightly different. Although the RDA for the first trimester remains the same as regular adults (0.8 grams per kilogram), the second and third trimester requires about 1.1 grams of protein per kilogram of body weight.
Furthermore, seafood consumption is highly recommended for pregnant women due to their positive association with young children’s cognitive development. Seafood is rich in healthy fats like Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).The recommendation is 8 to 12 ounces of various types of seafood that is low in methylmercury each week. High exposure to methylmercury is harmful to both the mother as well as the developing fetus.
Here are some of the best seafood choices (not an exhaustive list):
- Anchovy
- Atlantic mackerel
- Black sea bass
- Butterfish
- Catfish
- Clam
- Cod
- Haddock
- Salmon
- Oyster
- Sardine
- Shrimp
- Tilapia
- Canned tuna
- Lobster
On the other hand, here are the seafoods to avoid during pregnancy:
- King mackerel
- Marlin
- Orange roughy
- Shark
- Swordfish
- Tilefish (Gulf of Mexico)
- Tuna, bigeye
*From the FDA’s “Advice about eating fish”
Blood sugar balance and pcos
Insulin is a type of hormone that is secreted by the pancreas. When food is consumed, this hormone controls if the body wants to use or store the blood sugar. Previous studies have shown that with sufficient levels of insulin, protein does not increase blood sugar levels. This stabilizing effect was seen in patients with type 2 diabetes as well.
Furthermore there was also a study that suggested that a high protein diet is associated with lowering hemoglobin A1C levels (blood sugar level).
Studies have also shown that high protein and lower carbohydrate diets have led to a reduction in insulin resistance for women with Polycystic Ovary Syndrome (PCOS) who are also more prone to developing type 2 diabetes.
What are the high quality, high protein foods?
There are both animal and plant sources for protein.
Animal sources include meats, poultry, eggs, dairy and seafood. Plant sources include nuts, seeds, soy products, beans, peas, and lentils.
Processed and/or high-fat meats should be limited and instead fresh, frozen or canned forms of lean meat and poultry, seafood, and beans, peas, and lentils are recommended.
There is an increased interest in plant-based diets so here are some good plant-based protein sources:
- Dairy alternatives such as soy milk and fortified nut or pea milk
- Whole grains such as chickpea pasta, oatmeal, quinoa, or whole wheat bread
- Nuts and seeds such as almonds, hummus, peanut butter, tofu or chia seeds
- Vegetables such as broccoli, edamame, green peas or lima beans
The average American adult meets the required amount of protein consumption although this target is achieved (and even exceeded) mainly through animal based protein foods. Seafood and plant-based protein are categories that many Americans are lacking in.
Furthermore, despite the benefits that were mentioned in this article, it is important to keep in mind that more protein does not necessarily mean better. Overconsumption of protein has negative consequences as excess protein not only could get stored as fat but also could strain the kidneys as well.
Looking for more support?
If you would like more guidance as to what type of protein sources to incorporate in your diet as well as the adequate amount, check out our meal plans for more inspiration! We would love to support your journey.
References:
- “Advice About Eating Fish.” https://www.fda.gov/food/consumers/advice-about-eating-fish
- “Are You Getting Too Much Protein?” https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/are-you-getting-too-much-protein#:~:text=Extra%20protein%20intake%20also%20can,people%20predisposed%20to%20kidney%20disease.
- Murphy MM, Higgins KA, Bi X, Barraj LM. “Adequacy and Sources of Protein Intake among Pregnant Women in the United States, NHANES 2003–2012.” Nutrients. 2021 Mar; 13(3): 795. doi: 10.3390/nu13030795 PMCID: PMC7997328 PMID: 33670970
- Dietary Guidelines for Americans 2020-2025, https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf
- Dong J, Zhang Z, Wang P, Qin L. “Effects of High-protein Diets on Body Weight, Glycaemic Control, Blood Lipids and Blood Pressure in Type 2 Diabetes: Meta-Analysis of Randomised Controlled Trials.” Br J Nutr. 2013 Sep 14;110(5):781-9. doi: 10.1017/S0007114513002055. Epub 2013 Jul 5. PMID: 23829939
- Franz, MJ. “Protein: Metabolism and Effect on Blood Glucose Levels.” Diabetes Educ. 1997 Nov-Dec;23(6):643-6, 648, 650-1. doi: 10.1177/014572179702300603. PMID: 9416027
- Gannon MC, Nuttall JA, Damberg G, Gupta V, Nuttall FQ. “Effect of Protein Ingestion on the Glucose Appearance Rate in People with Type 2 Diabetes.” J Clin Endocrinol Metab. 2001 Mar;86(3):1040-7. doi: 10.1210/jcem.86.3.7263. PMID: 11238483
- “Insulin Basics”, https://diabetes.org/healthy-living/medication-treatments/insulin-other-injectables/insulin-basics
- Smith A, Colleen A, Spees C. “Wardlaw’s Contemporary Nutrition, 12th Edition.” McGraw Hill, 2022.
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook
