Resources
Style
Planning
View All
THE blog
Written by: Lauren Chamberlain
Edited and Reviewed By: Anabelle Clebaner MS, RDN
Hormonal contraceptives, including birth control pills, patches, injections, and intrauterine devices (IUDs), have transformed reproductive health, offering women reliable family planning options. However, many individuals experience symptoms after discontinuing hormonal contraception, a phenomenon sometimes referred to as post-birth control syndrome (PBCS). These symptoms can range from irregular cycles and acne to mood swings and digestive issues. Understanding the impact of hormonal contraceptives on the body and implementing strategies to support recovery can help ease this transition.
Understanding the Effects of Hormonal Contraceptives
Hormonal contraceptives work by suppressing ovulation, altering cervical mucus, and changing the uterine lining to prevent pregnancy. While effective, these changes influence several body systems, including the endocrine, digestive, and immune systems. Long-term use can disrupt the body’s natural hormone production, leading to potential withdrawal effects when stopping contraception.
A recent study found that hormonal contraceptives impact the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress response and hormone production. This may explain why some women experience mood disturbances and fatigue after discontinuation. Additionally, research suggests that birth control pills may alter gut microbiota composition, contributing to inflammation and digestive issues post-contraception.
The Role of the HPA Axis
The HPA axis plays a crucial role in regulating cortisol, a stress hormone that influences metabolism, immune function, and mood. Studies have shown that long-term contraceptive use can disrupt this delicate balance, leading to post-pill anxiety, fatigue, and even adrenal dysfunction. As the body readjusts, individuals may experience heightened stress sensitivity and emotional imbalances.
Additionally, research suggests that chronic hormonal suppression can contribute to reduced ovarian hormone production post-contraception, leading to symptoms like irregular cycles, low libido, and difficulty ovulating.
Common Symptoms After Stopping Hormonal Contraceptives
Post-birth control syndrome encompasses a variety of symptoms that may arise within weeks or months after stopping contraception.
Common symptoms include:
- Irregular or absent menstrual cycles
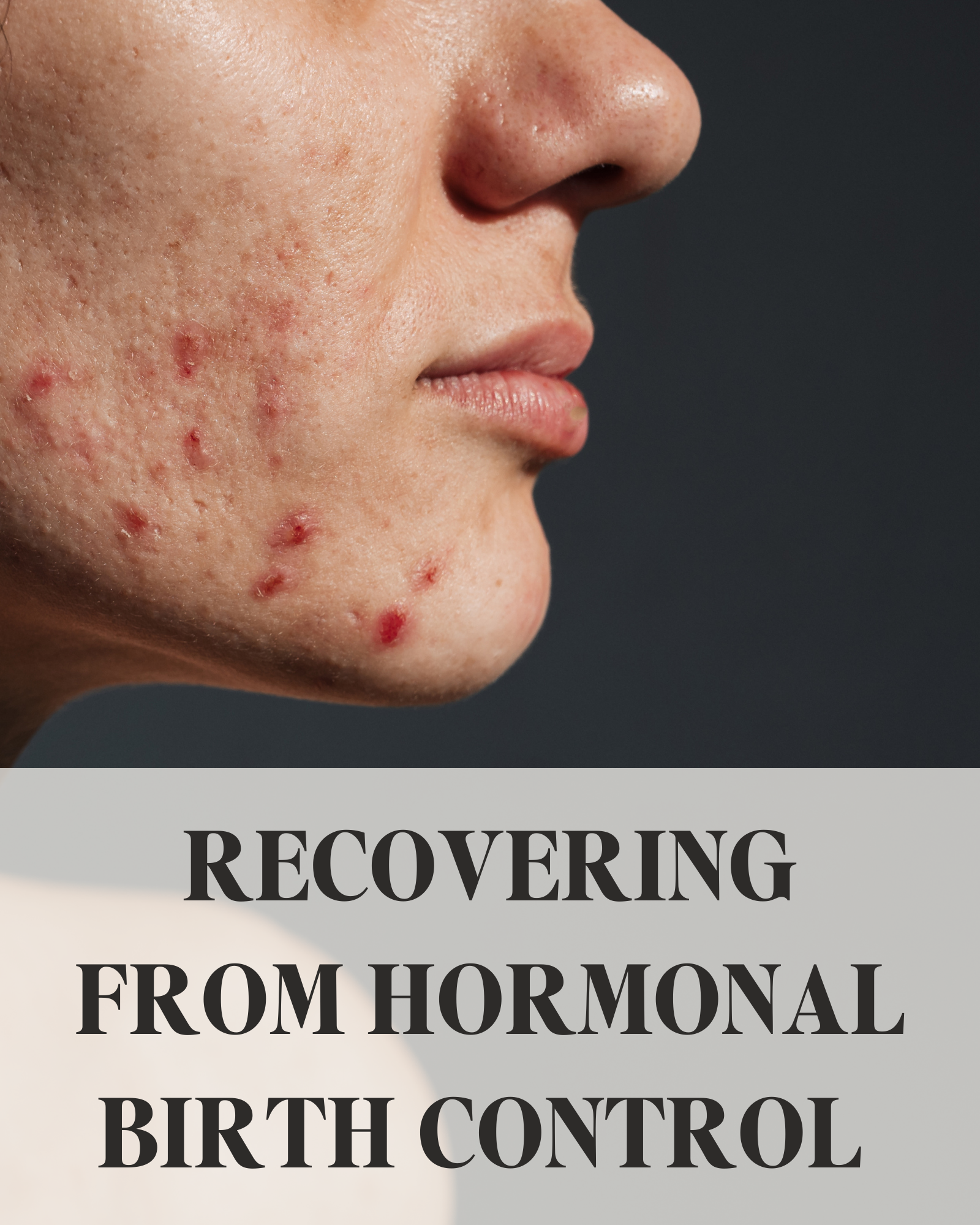
- Acne and skin changes
- Hair loss or thinning
- Digestive disturbances, including bloating and constipation
- Fatigue and mood swings
- Low libido
- Headaches and joint pain
These symptoms occur as the body attempts to restore natural hormone balance. For some, this transition is seamless, while for others, it may take several months to regulate.
Life After Birth Control: What to Expect
The transition off hormonal contraceptives varies for each individual. Some experience a smooth adjustment, while others face lingering hormonal imbalances.
- Menstrual Cycle Irregularities: It may take several months for cycles to regulate. If cycles remain absent or irregular for more than six months, professional evaluation is recommended. Ovulatory dysfunction is common post-contraception, particularly after long-term use of hormonal birth control. Tracking basal body temperature (BBT) and cervical mucus can provide insight into ovulation status and cycle health
- Acne and Skin Changes: Hormonal shifts can temporarily worsen acne. Supporting detox pathways, reducing dairy and sugar intake, and using non-comedogenic skincare products can help. Elevated androgens post-pill can contribute to excess sebum production, leading to breakouts. Incorporating zinc, omega-3 fatty acids, and antioxidants may promote clearer skin.
- Mood and Energy Levels: Some experience heightened anxiety or depression post-contraception. Prioritizing gut health, sleep, and stress reduction can ease this transition. The gut-brain axis plays a key role in mood regulation, making probiotics and a fiber-rich diet beneficial for mental well-being.
- Fertility Awareness: Some individuals regain fertility immediately, while others need time for ovulation to resume. Those trying to conceive may benefit from monitoring ovulation signs. If fertility does not return within six months, an evaluation for conditions like post-pill PCOS or hypothalamic amenorrhea may be necessary.
- Weight Fluctuations: Water retention and metabolism changes can impact weight. Focusing on whole foods, movement, and hydration supports a stable transition. Hormonal contraceptives can affect insulin sensitivity, and some women notice changes in blood sugar regulation post-pill. Balancing macronutrients and avoiding refined sugars can help stabilize weight.
- Increased Libido: Many report improved libido and natural cycle awareness after stopping hormonal contraceptives due to restored testosterone and estrogen levels.
Adjusting to life after birth control involves patience and self-care. Tracking symptoms, optimizing nutrition, and seeking support when needed can help individuals regain hormonal balance and overall well-being.
Supporting Hormonal Balance Post-Contraception
While post-birth control symptoms can be challenging, several strategies can support the body’s recovery and restore hormonal balance.
1. Nourishing Your Body with Key Nutrients
Hormonal contraceptives can deplete essential nutrients, including B vitamins, magnesium, zinc, and vitamin C. It has been found essential to replenish these nutrients to support metabolism, immune function, and hormone production.
Incorporating the following nutrient-dense foods can be beneficial:
- B Vitamins: Found in leafy greens, eggs, and whole grains
- Magnesium: Present in nuts, seeds, and dark chocolate
- Zinc: Found in oysters, beef, and lentils
- Vitamin C: Abundant in citrus fruits, bell peppers, and strawberries
Supplementing with a high-quality multivitamin or targeted nutrients may also help restore levels more efficiently.
2. Prioritizing Liver Health
The liver plays a crucial role in metabolizing hormones and detoxifying excess estrogen. Supporting liver function can aid hormone clearance and balance. Key strategies include:
- Drinking plenty of water to support detoxification
- Eating cruciferous vegetables (broccoli, cauliflower, kale) to promote estrogen metabolism
- Avoiding alcohol and excessive caffeine, which can burden the liver
- Taking liver-supporting supplements such as milk thistle and dandelion root
3. Balancing Blood Sugar Levels
Insulin resistance and blood sugar imbalances can contribute to hormonal dysregulation post-contraception. Stabilizing blood sugar helps maintain steady energy levels and prevents cortisol spikes, which can further disrupt hormones. To support blood sugar balance:
- Consume protein and healthy fats with every meal
- Avoid refined carbohydrates and excessive sugar
- Incorporate fiber-rich foods, such as legumes, nuts, and vegetables
- Engage in regular physical activity to improve insulin sensitivity
4. Restoring Gut Health
The gut microbiome influences hormone metabolism and immune function. Studies suggest that hormonal contraceptives may alter gut bacteria, leading to digestive issues and inflammation. Supporting gut health can enhance nutrient absorption and hormone clearance:
- Probiotic-Rich Foods: Yogurt, kimchi, sauerkraut, and kefir can replenish beneficial bacteria
- Prebiotic Fiber: Found in onions, garlic, bananas, and asparagus to support microbial diversity
- Bone Broth and Collagen: Aid in gut lining repair
- Limiting Processed Foods: Reducing inflammatory foods can alleviate digestive distress
- Fermented Foods and Fiber: Incorporating fermented foods like miso and fiber-rich foods such as flaxseeds can further support microbiome diversity
According to research, discontinuing birth control can cause shifts in the gut microbiome that affect estrogen metabolism and immune responses. A focus on gut healing post-contraception may accelerate hormonal recovery and reduce systemic inflammation.
5. Managing Stress and Prioritizing Sleep
Chronic stress and inadequate sleep can exacerbate hormonal imbalances. Since the HPA axis is affected by hormonal contraceptives, post-contraceptive recovery requires stress management techniques. Effective strategies include:
- Practicing mindfulness or meditation
- Engaging in gentle movement, such as yoga or walking
- Setting a consistent sleep schedule and avoiding blue light before bedtime
- Taking adaptogenic herbs, like ashwagandha or rhodiola, to support adrenal function
6. Tracking Your Menstrual Cycle
Monitoring menstrual patterns post-contraception provides insight into hormonal recovery. Using a cycle-tracking app or basal body temperature charting can help identify ovulation and cycle health.
- Basal Body Temperature (BBT): Measuring BBT each morning helps detect ovulation. A sustained temperature rise typically indicates ovulation has occurred.
- Cervical Mucus Changes: Observing cervical mucus consistency can signal fertility. Egg-white-like mucus usually indicates peak fertility.
- Cycle Length and Symptoms: Keeping track of cycle length, PMS symptoms, and flow characteristics provides valuable data about hormonal balance.
- Ovulation Predictor Kits: These kits measure luteinizing hormone (LH) surges, indicating the fertile window.
If menstruation does not return within three to six months, consulting a healthcare provider may be necessary to rule out underlying conditions like hypothalamic amenorrhea or PCOS.
7. Seeking Professional Support
If symptoms persist or become severe, working with a healthcare provider, such as a functional medicine/nutrition practitioner, can be beneficial. They can assess hormone levels, address underlying imbalances, and provide personalized recommendations for recovery.
Here are some issues you may need to address:
Prolonged Absence of Periods: If your period hasn’t returned after six months.
Persistent Acne or Severe Hair Loss: Significant changes in skin or hair health could indicate hormonal imbalances that require attention.
Excessive Mood Changes or Fatigue: If symptoms like mood swings, anxiety, or extreme tiredness persist.
Chronic Digestive Issues: Ongoing digestive disturbances such as bloating or constipation.
Conclusion
Recovering from hormonal contraceptives is a unique process for every individual. While some may transition smoothly, others may experience a range of symptoms as their body readjusts. By focusing on nutrient replenishment, liver and gut health, blood sugar balance, stress management, and cycle tracking, individuals can support their hormonal recovery more effectively. If challenges persist, seeking professional guidance can ensure a smoother transition and optimal long-term health.

Sources:
https://drbrighten.com/post-birth-control-syndrome
https://drbrighten.com/stopping-birth-control-side-effects
https://www.sciencedirect.com/science/article/pii/S0889159123003331?via%3Dihub
https://pmc.ncbi.nlm.nih.gov/articles/PMC6055351
https://drbrighten.com/the-contraception-guide/ https://www.kernodle.com/obgyn_blog/side-effects-of-stopping-the-pill-after-prolonged-use/
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook
