Resources
Style
Planning
View All
THE blog
Understanding PCOS: An Overview
Polycystic Ovary Syndrome (PCOS) is a multifaceted endocrine disorder that impacts a significant percentage of women during their reproductive years. Estimates suggest that PCOS affects between 4% to 18% of women worldwide, making it one of the most common hormonal disorders among women.
Characterized by a combination of symptoms, PCOS can vary widely from one individual to another. Common symptoms include irregular menstrual cycles, excessive hair growth (hirsutism), acne, and weight gain. Additionally, women with PCOS often face challenges related to insulin resistance, which can increase the risk of developing type 2 diabetes.
The exact cause of PCOS remains unclear. However, it is believed to be related to a combination of genetic and environmental factors. Hormonal imbalances, particularly an excess of androgens (male hormones that females also have), play a critical role in the development of PCOS symptoms.
Early diagnosis and management are key to mitigating the long-term health risks associated with PCOS. Common diagnostic tools include ultrasound imaging of the ovaries and blood tests to measure hormone levels. Despite its complexities, various lifestyle changes, such as diet and exercise, along with medical treatments, can help manage the condition effectively.
Understanding the intricacies of PCOS not only empowers you with knowledge but also offers a pathway to improving your overall health and well-being. With the right approach, you can manage the symptoms and live a fulfilling life.
Why Supplements Matter in Managing PCOS
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting millions of women worldwide. Symptoms such as irregular menstrual cycles, weight gain, acne, and excessive hair growth can significantly impact your quality of life. Supplements can play a crucial role in managing these symptoms effectively.
Addressing Nutrient Deficiencies: Many women with PCOS are found to be deficient in essential vitamins and minerals like Vitamin D, Magnesium, and Zinc. These deficiencies can exacerbate symptoms, making it more challenging to manage the condition. By supplementing these nutrients, you can help restore balance and support your overall health.
Hormonal Regulation: PCOS often leads to hormonal imbalances, particularly with insulin and androgens. Supplements such as Inositol and Omega-3 Fatty Acids have been shown to aid in regulating these hormones, thereby reducing symptoms like acne and excessive hair growth. Inositol, for instance, has been found to improve insulin sensitivity, which is crucial for managing PCOS.
Reducing Inflammation: Chronic inflammation is a common issue in women with PCOS, contributing to insulin resistance and other metabolic problems. Omega-3 Fatty Acids are well-known for their anti-inflammatory properties and can help reduce systemic inflammation, improving your overall metabolic health.
Improving Mental Well-being: Living with PCOS can take a toll on your mental health, leading to stress and anxiety. Supplements like Magnesium not only help with physical symptoms but also support mental well-being by promoting relaxation and better sleep. Improved sleep and reduced stress can significantly impact how you manage your PCOS symptoms day-to-day.
Ultimately, while supplements are not a cure-all for PCOS, they can be a valuable part of a comprehensive management strategy. Always consult with a healthcare professional to create a tailored supplement plan that addresses your specific needs and conditions. Taking the right supplements can help you take control of your health and mitigate the challenges posed by PCOS.
Vitamin D: The Sunshine Vitamin for Hormonal Balance
Vitamin D, often referred to as the sunshine vitamin, plays a crucial role in maintaining hormonal balance, especially for those grappling with PCOS. Many individuals with PCOS are found to have a deficiency in Vitamin D, which can compound the condition’s already complex symptoms. But what exactly makes this vitamin so vital?
Firstly, Vitamin D acts like a hormone itself, impacting the function of over 200 genes, including those involved in the regulation of the menstrual cycle and reproduction. Research has shown that adequate levels of Vitamin D can help improve insulin sensitivity, which is often a significant concern for individuals with PCOS. In essence, better insulin sensitivity can lead to more balanced blood sugar levels and reduced symptoms.
Moreover, Vitamin D also supports healthy pregnancies. Ensuring optimal levels can make a big difference for women with PCOS trying to conceive, as it helps in the regulation of menstrual cycles and the maintenance of healthy hormone levels.
So, whether you’re soaking up the sun or considering a supplement like HUM’s Here Comes the Sun Vitamin D3, incorporating this vitamin into your routine can profoundly impact your journey towards hormonal balance and overall well-being.
Inositol: A Natural Approach to Hormone Regulation
Inositol, often referred to as Vitamin B-8, plays a crucial role in managing PCOS symptoms by naturally regulating hormone levels. There are two main forms that are particularly effective for women with PCOS: Myoinositol and D-chiro-inositol.
Both forms have been shown to improve insulin-receptor activity, which can be beneficial in reducing insulin resistance—a common issue for those with PCOS. Enhanced insulin sensitivity helps to stabilize blood sugar levels and may mitigate some of the hormonal imbalances that characterize this condition.
Additionally, a combination of inositol derivatives and alpha-lipoic acid (ALA) has been demonstrated to further improve insulin sensitivity, support ovulatory function, and reduce hyperandrogenism. Hyperandrogenism, signified by elevated levels of male hormones, often leads to symptoms like hirsutism (excessive hair growth) and acne. By addressing these symptoms, inositol can contribute significantly to a better quality of life for women suffering from PCOS.
If you’re considering inositol as a supplement, it’s important to note its potential benefits aren’t limited to insulin regulation. Research suggests that inositol can help balance several other hormones related to reproductive health, offering a holistic approach to managing PCOS symptoms. This makes inositol a versatile and promising option worth discussing with your healthcare provider.
Omega-3 Fatty Acids: Reducing Inflammation and Insulin Resistance
Omega-3 fatty acids, typically found in fish oil, play a pivotal role in managing PCOS symptoms. One of their standout benefits is their ability to reduce inflammation, which is often at the crux of many PCOS-related issues. By lowering inflammation, omega-3s help to mitigate the systemic stress that can exacerbate hormonal imbalances.
But the benefits don’t stop there. Omega-3s are also known for their positive effect on insulin resistance—a common concern for those with PCOS. Insulin resistance occurs when cells in your muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from your blood. By improving insulin sensitivity, omega-3s aid in maintaining more stable blood sugar levels, which is crucial for managing PCOS effectively.


Research suggests that regularly incorporating omega-3s can help balance lipid levels, improving overall metabolic health. This can be particularly beneficial for those with PCOS, who often face challenges related to weight management and cardiovascular health. The anti-inflammatory properties of omega-3s make them a valuable addition to your supplement regimen, especially when you are aiming to tackle the multi-faceted challenges of PCOS.
For the best results, consider adding sources of omega-3s such as fatty fish (like salmon, mackerel, and sardines) to your diet, or opt for high-quality fish oil supplements. Aim for a balanced intake to harness the full spectrum of benefits that omega-3s offer. Always consult your healthcare provider before starting any new supplement to ensure it’s right for you.
Magnesium: Combatting Stress and Improving Sleep
Magnesium plays a pivotal role in managing PCOS by aiding in stress reduction and enhancing sleep quality. This mineral is known for its natural calming effect, which can help mitigate the elevated stress levels often experienced by those with PCOS. Elevated stress can exacerbate PCOS symptoms, making magnesium supplementation particularly beneficial.
Moreover, magnesium supports proper blood sugar regulation, a critical factor for managing PCOS. This nutrient’s ability to enhance insulin sensitivity can help maintain stable blood sugar levels, potentially reducing the risk of insulin resistance—a common challenge for many with PCOS.
When it comes to improving sleep, magnesium is a game-changer. It helps regulate neurotransmitters that send signals to the brain and nervous system, creating a more conducive environment for restful sleep. Poor sleep quality can significantly impact hormone levels, worsening PCOS symptoms. By improving sleep, magnesium indirectly supports hormonal balance.

Not all magnesium supplements are created equal. Magnesium Bisglycinate is often recommended for its superior absorption and minimal digestive discomfort compared to other forms. Including this specific form of magnesium in your routine may offer the best results in combating stress, regulating blood sugar, and improving sleep quality.
Incorporating magnesium-rich foods into your diet, such as leafy greens, nuts, seeds, and whole grains, can further bolster your magnesium intake. Nevertheless, a supplement can ensure you consistently meet your daily needs, providing a robust foundation for managing PCOS symptoms effectively.
Zinc: Supporting Reproductive Health
Zinc is an essential trace mineral that plays a pivotal role in many bodily functions, including immune response, DNA synthesis, and cell division. When it comes to managing PCOS, zinc shines particularly in supporting reproductive health.
Studies have demonstrated that zinc supplementation can improve fertility and enhance reproductive function. This is particularly crucial for those with PCOS, as hormonal imbalances often lead to irregular menstrual cycles and ovulation issues. By helping to regulate the hormonal environment, zinc can promote regular ovulation and menstrual regularity, increasing the chances of conception.
In addition, zinc’s antioxidant properties help combat oxidative stress, which is often elevated in individuals with PCOS. Oxidative stress can cause cellular damage and inflammation, further complicating PCOS symptoms. By reducing oxidative stress, zinc contributes to a healthier reproductive system and overall well-being.

Considering the different forms of zinc supplements available, such as zinc sulfate and zinc picolinate, it’s important to choose a form that offers high bioavailability. Zinc picolinate is often recommended because it’s easily absorbed by the body, ensuring you get the maximum benefits.
Before starting any new supplement regimen, it’s wise to consult with a healthcare provider to determine the appropriate dosage and to ensure it aligns with your individual health needs. Integrating zinc into your supplement routine might just be the step you need to better manage your PCOS and support your reproductive health.
NAC – N- Acetyl-Cysteine
- Antioxidant: NAC can help restore the balance of antioxidants and inflammatory markers in women with PCOS.
- Ovulation: NAC can increase ovulation and pregnancy rates.
- Insulin: NAC may be an alternative to other insulin-lowering drugs like metformin, and may help with hyperinsulinemia in women with PCOS.
- Sex hormones: NAC can reduce testosterone levels and increase follicle-stimulating hormone (FSH) levels.
- Metabolic parameters: NAC may improve metabolic parameters in women with PCOS.
In addition to these benefits, NAC is recognized for its role in detoxification. As a precursor to glutathione, one of the body’s most powerful antioxidants, it supports the liver in removing toxins and free radicals, helping to maintain a healthy internal environment. Another noteworthy aspect is its potential in enhancing mood and mental well-being. Women with PCOS often experience mood swings and mental health issues. NAC has been studied for its positive effects on mental health, such as alleviating symptoms of anxiety and depression, thanks to its ability to regulate glutamate levels and its antioxidative properties. When looking to add NAC to your supplement regime, it’s crucial to speak with a healthcare provider first. While NAC can offer significant benefits, it’s always best to ensure it’s the right fit for your specific health needs and circumstances, especially when dealing with a complex condition like PCOS.
Herbal Allies: The Role of Spearmint and Cinnamon
When it comes to managing PCOS, nature has some incredible allies. Two standout herbs that have shown promising results are spearmint and cinnamon. These herbal allies bring more to the table than delightful flavors; they offer real benefits for women battling the symptoms of PCOS.

Spearmint: Known for its refreshing taste and aroma, spearmint has been traditionally used for its soothing properties. But did you know it also boasts significant anti-androgen effects? Studies have shown that drinking spearmint tea can help reduce elevated androgen levels, which are often responsible for unwanted symptoms like hirsutism (excessive hair growth) in women with PCOS. Consider adding Traditional Medicinals Organic Spearmint Tea to your daily routine for a natural way to support hormonal balance. Cinnamon: This well-loved spice is more than just a kitchen staple; it’s a potent tool for improving menstrual cyclicity and reducing insulin resistance. Preliminary research indicates that cinnamon can help regulate menstrual cycles in women with PCOS, making it a valuable ally in managing the condition. A pilot study also highlights cinnamon’s potential to improve parameters of insulin resistance, which is a common issue for those with PCOS.
Incorporating these herbal allies into your daily diet doesn’t have to be complicated. Enjoy a cup of spearmint tea in the afternoon, or add a sprinkle of cinnamon to your morning oatmeal or smoothies. These simple additions can make a significant difference in managing PCOS symptoms naturally.
How to Choose Quality Supplements for PCOS
Selecting the right supplements can be a game-changer in managing PCOS. However, it’s crucial to choose high-quality supplements to ensure safety and efficacy. Here are some tips to help you make informed choices:
Look for supplements that have been tested by an independent third party. Certifications such as NSF International, USP (United States Pharmacopeia), or ConsumerLab can provide added assurance of quality and purity.
Check out my Fullscript store for medical-grade supplements.
Combining Diet and Supplements for Optimal Results
Pairing the right supplements with a thoughtfully planned diet can significantly enhance your efforts in managing PCOS. It’s all about synergy – the way certain foods and supplements work together to amplify their benefits.
Focus on Whole Foods: Start with a diet rich in whole foods like fresh fruits, vegetables, lean proteins, and whole grains. These foods provide essential nutrients and fiber, which aid in stabilizing blood sugar levels and improving overall health.
Balance Your Nutrients: Incorporate foods that are high in the key nutrients found in your supplements. For instance, fatty fish like salmon can boost your intake of Omega-3 fatty acids, while leafy greens and nuts can enhance your magnesium levels. Balancing your diet this way ensures you’re getting a wide spectrum of nutrients while maximizing the impact of your supplements.
Consider Anti-Inflammatory Foods: Chronic inflammation is a common issue in PCOS. Introduce anti-inflammatory foods such as turmeric, ginger, and berries to your diet. These not only complement the action of supplements like Omega-3s but can also help in reducing overall inflammation and improving insulin sensitivity.
Limit Processed Foods and Sugars: Reducing the intake of processed foods and sugars is crucial. These can exacerbate insulin resistance and hormonal imbalances, counteracting the benefits of your supplements. Opt for natural sweeteners and whole food alternatives wherever possible.
Stay Hydrated: Hydration is often overlooked but is essential for overall health and well-being. Drinking plenty of water helps in the effective absorption of supplements and assists in maintaining metabolic processes crucial for managing PCOS.
Monitor and Adjust: Everyone’s body responds differently, so it’s important to monitor how you’re feeling and make adjustments as needed. Keep a food and supplement journal to track what works best for you and discuss these observations with your healthcare provider.
Combining a well-rounded, nutrient-dense diet with carefully selected supplements can create a powerful strategy for managing PCOS. Remember, there’s no one-size-fits-all approach – it’s about finding the right balance that works for your body.

The Connection Between Blood Sugar and Hormone Health
Your hormonal health is intricately linked to your blood sugar levels, primarily through the action of insulin. Insulin is a hormone produced by the pancreas that regulates glucose levels in the blood. When you consume foods high in sugar or refined carbohydrates, your blood sugar levels spike. In response, your body releases insulin to help absorb that glucose into cells for energy. However, frequent spikes can lead to insulin resistance, a condition where cells become less responsive to insulin, causing imbalances.
These imbalances can disrupt the delicate interplay of other hormones like estrogen and progesterone, which are crucial for fertility. For instance, polycystic ovary syndrome (PCOS), a common endocrine disorder affecting women of reproductive age, is strongly correlated with insulin resistance and high blood sugar levels. Managing your blood sugar through a balanced diet, regular exercise, and stress management can support hormone health, thus enhancing fertility prospects.
Moreover, ensuring stable blood sugar levels is not only vital for your hormonal balance but also for preventing potential complications during pregnancy. Higher blood glucose levels can lead to gestational diabetes, posing risks to both you and your baby. Therefore, understanding and managing blood sugar is a fundamental step toward achieving and maintaining hormonal health, ultimately supporting your journey towards conception.
Breakfast: Kickstart Your Day with Fertility-Boosting Foods
Breakfast is indeed the most important meal of the day, especially when you’re focusing on enhancing fertility. A nutrition-packed breakfast can set the tone for the entire day, stabilizing blood sugar levels and providing essential nutrients for hormone balance. But what exactly should you be eating?
Start with whole grains. Foods like oatmeal, quinoa, or whole-grain toast are excellent choices as they offer a slow release of energy, preventing those mid-morning energy dips. Pair these with a source of protein such as eggs, Greek yogurt, or a plant-based alternative like tofu. Protein supports the production of crucial fertility hormones and helps maintain stable blood sugar levels.
Don’t forget the healthy fats! Avocado, nuts, and seeds are not only delicious additions but also help in the absorption of fat-soluble vitamins. These vitamins play a significant role in hormone production and balance.
A great example of a fertility-boosting breakfast could be a bowl of oatmeal topped with chia seeds, fresh berries, and a dollop of almond butter. This meal hits all the right notes with complex carbohydrates, protein, and healthy fats, keeping you full and energized throughout the morning.
Additionally, incorporating a serving of colorful fruits or vegetables can provide an array of vitamins, minerals, and antioxidants. These nutrients are essential for protecting your cells from damage and supporting overall reproductive health. Try adding a handful of spinach to your morning smoothie or enjoying a side of mixed fruit with your eggs.
Remember, consistency is key. Regularly consuming a balanced breakfast can significantly impact your blood sugar levels and hormone health over time, making it a cornerstone of your fertility journey.
Lunch: Building a Balanced Plate for Optimal Fertility
Lunch is a pivotal moment in your day, offering an excellent opportunity to refuel with nutrient-dense foods. Balancing your plate not only satisfies hunger but also stabilizes blood sugar levels—a key factor for hormone health and fertility. How can you craft the perfect meal? Follow the ‘Plate Method’ for simplicity and effectiveness.
- Fill Half Your Plate with Non-Starchy Vegetables: These veggies are packed with vitamins, minerals, and antioxidants crucial for reproductive health. Think leafy greens like spinach, kale, and arugula, or colorful choices such as bell peppers, tomatoes, and carrots.
- One Quarter Lean Protein: Protein is essential for hormone production and repairing bodily tissues. Options include grilled chicken, turkey, tofu, or legumes such as lentils and chickpeas. Aim for around 20-30 grams of protein per meal to meet your daily needs.
- One Quarter Whole Grains or Complex Carbohydrates: These carb sources, like quinoa, brown rice, or whole-grain bread, provide steady energy and help maintain stable blood sugar levels. They also offer fiber, which supports digestive health and hormone balance.
To take your lunch to the next level, incorporate healthy fats like avocado slices, olive oil dressings, or a sprinkle of seeds. Healthy fats are crucial for hormone production and keeping you feeling satisfied.
Here’s a quick and delicious lunch idea to get you started:
Quinoa Salad with Grilled Chicken: Combine cooked quinoa with mixed greens, cherry tomatoes, and cucumber slices. Top with grilled chicken breast and a handful of chickpeas. Drizzle with a simple olive oil and lemon juice dressing, and sprinkle some sunflower or pumpkin seeds.
This meal is not only tasty but also packed with the nutrients you need to support your fertility journey.
Afternoon Snack: Satisfy Cravings and Stabilize Blood Sugar
An afternoon snack is more than just a mini-meal; it’s a strategic opportunity to maintain your blood sugar levels and keep your energy steady throughout the day. The key to a balanced snack is combining carbohydrates with protein and healthy fats. This combination helps to slow the absorption of sugar into your bloodstream, preventing the spikes and crashes that can disrupt your insulin levels and hormone balance.
Example Snack Ideas:
- Apple Slices with Almond Butter: The fiber in the apple pairs perfectly with the protein and healthy fats in almond butter to keep you full and satisfied.
- Greek Yogurt with Berries: A high-protein option that also provides antioxidants and fiber from the berries. Choose unsweetened yogurt to avoid added sugars.
- Hummus with Veggie Sticks: Carrot sticks, cucumber slices, or bell pepper strips dipped in hummus offer a satisfying crunch along with protein and healthy fats from the chickpeas and tahini.
- Whole-Grain Crackers with Cheese: Opt for whole-grain crackers to stabilize blood sugar and pair them with a small piece of cheese for protein and fat.
When planning your afternoon snack, remember to portion wisely. Overeating can lead to an insulin spike, which is counterproductive to your goals. Aim for about 150-200 calories, and listen to your body’s hunger cues. This habit will not only help you get through the afternoon slump but also contribute positively to your overall fertility journey.
Dinner: Delicious and Nutritious Meals to Support Conception
As you wind down your day, dinner presents the perfect opportunity to savor a meal that not only satisfies but also supports your fertility. A balanced dinner should focus on lean proteins, healthy fats, fiber-rich vegetables, and whole grains to keep your blood sugar stable throughout the night.
Consider starting with a grilled salmon filet, which is rich in omega-3 fatty acids known to enhance fertility. Pair this with a generous helping of quinoa salad, packed with fiber, protein, and essential vitamins. To round out your meal, add a side of roasted Brussel sprouts tossed with olive oil, garlic, and a sprinkle of sea salt for an extra nutrient boost.
If you’re vegetarian, you might opt for a hearty lentil stew. Lentils are a great plant-based protein source and are high in folate, an essential nutrient for prenatal health. Combine your stew with a side of steamed asparagus, which provides vitamins A and C, and top it with a squeeze of fresh lemon juice for added flavor and vitamin C.
Don’t forget to include healthy fats in your dinner. Adding a drizzle of extra virgin olive oil to your salad or vegetables can enhance the absorption of fat-soluble vitamins. An avocado salad is another fantastic option, offering monounsaturated fats that support hormone production.
Remember, the goal of this meal is to load up on nutrient-dense foods that will support both your blood sugar levels and reproductive health. Bon appétit!
Dessert: Healthy Sweet Treats That Won’t Spike Your Blood Sugar
When cravings for something sweet hit, it’s important to make mindful choices that won’t send your blood sugar levels soaring. Luckily, there are delicious and nutritious options that satisfy your sweet tooth without sacrificing your fertility goals.
Opt for fruit-forward desserts that bring natural sweetness and a host of nutrients. For instance, fresh berries with a dollop of Greek yogurt or a sprinkle of nuts make a perfect end to any meal. Not only do these options provide fiber, but they also offer protein and healthy fats, which help stabilize blood sugar levels.
If you’re craving something baked, consider preparing a batch of oat-based cookies sweetened with just a touch of honey or maple syrup. Using whole grains like oats ensures that your body digests the carbohydrates more slowly, avoiding the rapid blood sugar spikes caused by refined grains and simple sugars.
Another tasty option is chia pudding. Mix chia seeds with unsweetened almond milk and a bit of vanilla extract. Let it sit overnight, allowing the seeds to absorb the liquid and turn into a creamy, satisfying dessert. Top with fresh fruit for added flavor and nutrition. This dessert not only provides fiber but also omega-3 fatty acids, great for hormone health.
Keep sweets like soft drinks and pastries to a minimum or avoid them altogether. These foods are high in sugar and offer little nutritional value, which can counteract your efforts to manage blood sugar and support fertility.
Remember, the aim is to indulge in a way that aligns with your health goals. By choosing nutrient-rich, lower-glycemic options, you can enjoy a sweet treat while keeping your blood sugar levels stable and supporting your journey towards conception.
Hydration: The Role of Fluids in Blood Sugar and Fertility
Staying hydrated is vital for maintaining balanced blood sugar levels, which directly impacts your fertility. Water is crucial in facilitating the transportation of nutrients to your cells, and ensuring that your body can efficiently eliminate waste. When it comes to hydration, you want to be mindful of both the quantity and quality of the fluids you consume.
Why water is your best friend: Water keeps your blood volume at the appropriate level, which helps in better regulation of insulin and blood sugar levels. It also helps to reduce the risk of bloating and water retention, making you feel more comfortable and energized throughout the day.
But how much water should you drink? The general recommendation is to aim for at least eight 8-ounce glasses a day, but this can vary based on your activity level, the climate you live in, and your overall health. A handy tip is to always carry a reusable water bottle with you, so you can sip throughout the day and keep track of how much you’re drinking.
Beverages to avoid: While it’s important to stay hydrated, not all fluids are created equal. Beverages high in sugar, such as sodas and fruit juices, can cause sudden spikes in blood sugar levels, which are detrimental to both your blood sugar balance and your fertility. Similarly, excessive caffeine consumption can lead to dehydration. Try to limit your intake of caffeinated drinks and opt for decaf versions or herbal teas instead.
Conclusion
Your daily meal plan is more than a dietary choice; it’s a strategic approach to health and fertility. By intentionally balancing blood sugar levels throughout the day, you are not only nurturing your body’s overall well-being but also optimizing your reproductive health. Each meal, from breakfast to dessert, plays a vital role in stabilizing blood glucose and supporting hormonal health, which are both essential for conception.
Remember, small changes can make a big difference. Incorporating a variety of nutrient-dense foods, rich in fiber, protein, and healthy fats, helps maintain steady blood sugar levels. This, in turn, reduces inflammation and supports hormone health, creating a more favorable environment for fertility.
Hydration also cannot be overlooked. Fluids are crucial for maintaining blood sugar levels and supporting every function of your body, including fertility. Aim to drink plenty of water throughout the day, and consider adding herbal teas that may offer additional fertility benefits.
As you embark on this journey, consider keeping a food journal to track your progress and notice how different foods affect your blood sugar and overall wellness. Additionally, consult with a healthcare provider or nutritionist who can offer personalized guidance and support tailored to your specific needs.
By making mindful choices and prioritizing balanced meals, you are taking proactive steps toward enhancing your fertility and well-being. Here’s to a nourishing and hopeful path to conception!
Looking for More Support?
Check out our popular four week fertility meal plan filled with blood sugar balanced meals right here.
Are you struggling with low progesterone levels and wondering how to boost them naturally? You’re not alone. Progesterone is a crucial hormone for women, playing an essential role in the menstrual cycle and maintaining pregnancy. Low levels can lead to a variety of health issues, including irregular periods, mood swings, and fertility challenges. Fortunately, there are natural ways to raise progesterone levels and improve your overall well-being.
In this article, we’ll explore the best natural strategies to increase your progesterone, covering key areas such as diet, stress management, herbal supplements, and more. Follow our tips and advice, and take proactive steps towards balancing your hormones naturally.
What is progesterone?
Progesterone is a hormone that is secreted by the corpus luteum in your ovary in the second half of your menstrual cycle after you ovulate. A small amount of progesterone is also made by your adrenal glands & if you’re pregnant, your placenta will eventually make most of the progesterone.
Progesterone’s main role in the body is to help prepare the lining of your uterus for a possible pregnancy. If you don’t become pregnant, your progesterone levels begin to drop & you have your period. If you do conceive, progesterone continues being produced & helps to further prepare your uterus so that the fertilised egg can implant successfully & your pregnancy can be maintained.
Progesterone is produced primarily by your ovaries following ovulation, but it’s also made in smaller quantities by the adrenal glands. This hormone works alongside estrogen to ensure that your menstrual cycle proceeds smoothly. In addition to its reproductive functions, progesterone plays a role in regulating mood, contributing to a sense of well-being, and even aiding in cognitive function.
When progesterone levels are low, you may experience a range of symptoms, including irregular menstrual cycles, mood swings, and difficulties with conception. It’s crucial to maintain balanced hormone levels to support not only your reproductive health but also your overall well-being.
Interestingly, men also produce progesterone, albeit in smaller amounts. In both men and women, this hormone helps to balance the effects of estrogen, making it a vital component of hormonal health.
Understanding how to naturally increase your progesterone levels can make a significant difference, especially if you’re dealing with symptoms that might indicate a deficiency. From dietary changes to lifestyle adjustments, there are several natural methods you can employ to raise your progesterone levels effectively.
Signs of low progesterone

When you don’t ovulate, or only produce small amounts of progesterone after ovulation, you might have some of the following symptoms:
- Irregular or absent periods⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Abnormal bleeding or spotting⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Recurrent miscarriages⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Decreased sex drive ⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Weight gain⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Migraines or headaches⠀⠀⠀⠀⠀⠀⠀⠀⠀
- Mood changes ⠀⠀⠀⠀⠀
In addition to the symptoms listed above, low progesterone levels can lead to:
- Hot flashes and night sweats
- Fluid retention or bloating
- Sagging skin and wrinkles
- Fatigue and difficulty concentrating
- Increased PMS symptoms
- Breast tenderness
If you experience these symptoms, it’s essential to seek medical advice. Your healthcare provider can offer tailored guidance and interventions to help balance your hormones and alleviate symptoms.
What causes low progesterone?
Low progesterone due to anovulation or irregular ovulation is one of the most common reasons for low progesterone levels & this is why low progesterone can be common in conditions such as Polycystic Ovary Syndrome (PCOS). There can be a number of reasons why your progesterone levels might be low so it’s always important to see a medical doctor for full investigations.
Addressing the root cause of low progesterone often involves lifestyle changes and natural interventions. Incorporating these changes not only helps boost progesterone levels but also improves overall well-being.
Stress management is crucial since chronic stress can hinder progesterone production. Techniques such as yoga, meditation, and regular physical activity can significantly reduce stress levels. Similarly, maintaining a healthy weight also plays a key role, as both low and high body weight can disrupt hormonal balance.
Equally important is avoiding exposure to endocrine disruptors—substances that mimic estrogen and can further throw off your hormonal balance. These can be found in many everyday products, including certain plastics, personal care items, and even some food sources.
Taking a holistic approach by focusing on a nutrient-rich diet, stress management, and a healthy lifestyle can create a conducive environment for your body to balance its hormones naturally. For persistent or severe cases, it’s crucial to consult a healthcare provider who can offer targeted treatments and interventions.
How to increase progesterone naturally
1. How to increase progesterone naturally: Nutrient-Rich Diet
Your diet plays a crucial role in supporting progesterone production. Focus on consuming foods rich in:
- Vitamin B6: Found in lean meats, fish, bananas, and potatoes, Vitamin B6 helps the body produce progesterone. Vitamin B6 is a nutrient that is involved in making cells & hormones, including the hormone progesterone. One study found that Vitamin B6 supplementation helped to reduce estrogen & increase progesterone levels. Another study found that A diet rich in vitamin B6 can increase progesterone levels by up to 30%
- Magnesium: Essential for many of the body’s processes, magnesium is found in leafy greens, nuts, seeds, and whole grains.
- Zinc: Nuts, seeds, beef, and shellfish are excellent sources of zinc, which supports progesterone production.
- Vitamin E: has been shown to increase luteal blood flow, which lengthens the luteal phase. It has also been shown to improve the corpus luteum—it dictates how much progesterone we produce each cycle and can mitigate effects of excess estrogen. (If you’re looking for a vitamin E supplement, look for one that has mixed tocopherols like this one)
- Vitamin C: Vitamin C is also a powerful antioxidant & emerging research shows that Vitamin C intake is linked with higher progesterone levels.
Omega-3 fats: Omega-3 fatty acids can enhance progesterone production by 20% – found in foods like fatty fish and walnuts.

2. How to increase progesterone naturally: Manage Stress
Stress can deplete progesterone levels since high stress prompts the body to produce more cortisol (a stress hormone), often at the expense of progesterone. Techniques such as yoga, meditation, and even regular physical activity can help manage stress levels effectively.
3. How to increase progesterone naturally: Herbal Supplements
Certain herbs have been traditionally used to support hormone balance, including:
- Chasteberry (Vitex agnus-castus): Thought to support the production of progesterone by encouraging the pituitary gland to produce more luteinizing hormone (LH). Herbal supplements like chasteberry can boost progesterone levels by 15%
- Maca Root: Often used to balance estrogen and progesterone levels.
- Evening Primrose Oil: Known for its potential in balancing hormones, which can indirectly support healthy progesterone levels.
4. How to increase progesterone naturally: Maintain a Healthy Weight
Excess body fat can lead to increased estrogen levels, which may disrupt the balance with progesterone. Aim for a balanced diet and regular exercise to maintain a healthy weight.
Either not having enough body fat or a having a body fat percentage that is too high can impact on ovulation & your bodies ability to produce progesterone naturally. Having a higher body weight makes you three times more likely to struggle with irregular periods. If you’re weight is either too low or higher than ideal, it might be worth speaking with one of our fertility dietitians about how you can optimize your weight in a healthy, sustainable way that will enhance your fertility, not decrease it.
5. How to increase progesterone naturally: Avoid Estrogen Mimickers
Minimize your exposure to xenoestrogens, which are synthetic compounds that mimic estrogen in the body. These can be found in some plastics, personal care products, and pesticides. Opt for natural and organic options whenever possible.
Incorporating these strategies into your lifestyle can help you naturally boost your progesterone levels, leading to improved overall health and well-being. Always consult with a healthcare professional before making any significant changes, especially if you have underlying health conditions or are on medication.
6. How to increase progesterone naturally: Ovulate regularly
One of the best ways to naturally increase progesterone is to focus on diet & lifestyle strategies to support healthy, strong & regular ovulation.
Nutrition & lifestyle strategies that can help support you ovulate regularly & have a regular period include:
- Choosing good quality, low GI carbs
- Reducing your glycemix load & eating the right amount of carbohydrates for your individual needs
- Increasing your intake of foods rich in omega 3 fats & reducing your intake of foods high in saturated & trans fats
- Eating enough calories for your individual needs & avoiding restrictive diets
- Reviewing & reducing your alcohol intake
- Reducing stress
- Prioritising adequate sleep
How Stress Affects Progesterone and How to Manage It
When you’re stressed, your body releases cortisol, also known as the stress hormone. While cortisol is essential for managing stress, chronic high levels can disrupt the balance of other crucial hormones, including progesterone. Essentially, your body prioritizes cortisol production over progesterone, leading to a condition often referred to as “progesterone steal.”
Managing stress effectively is vital for maintaining healthy progesterone levels. In fact, stress reduction techniques can lead to a 25% improvement in progesterone levels
Here are some actionable strategies:

Practice Mindfulness and Meditation
Mindfulness practices such as meditation and deep breathing exercises can significantly reduce stress levels. This, in turn, can help keep your hormone levels balanced. Start with just a few minutes a day and gradually increase the duration as it becomes a natural part of your routine.
Engage in Regular Physical Activity
Exercise is a great stress reliever, but it’s important to strike the right balance. Moderate activities like walking, yoga, or swimming can help reduce stress without overtaxing your body. Avoid overexercising, as it can increase cortisol levels and negatively impact progesterone production.
Ensure Adequate Sleep
Quality sleep is crucial for hormone regulation. Aim for 7-8 hours of uninterrupted sleep per night – Women who sleep 7-8 hours per night have a 10% higher progesterone level on average. Creating a calming bedtime routine, such as turning off screens an hour before bed and practicing relaxation techniques, can promote better sleep quality.
Connect with Loved Ones
Social support is a powerful stress buffer. Spending time with friends and family can elevate your mood and reduce stress levels. Whether it’s through a phone call, video chat, or a face-to-face meeting, make sure to stay connected with your support network.
Conclusion
Understanding how to naturally increase progesterone levels can have a profound effect on your overall well-being. By incorporating a nutrient-rich diet, managing stress effectively, considering herbal supplements, and maintaining a healthy weight, you can support your body’s hormonal balance.
Additionally, avoiding estrogen mimickers and striving for regular ovulation further boost your progesterone levels. Remember, small, consistent changes often lead to the most sustainable results. Prioritize your health, listen to your body, and don’t hesitate to seek professional guidance if needed. With dedication and the right approach, you can achieve a harmonious hormonal balance naturally.
Looking for More Support?
If you’re struggling with hormonal imbalances like low progesterone, reach out to our team of trained fertility dietitians. We help women balance their hormones naturally using a combination of nutrition therapy, functional lab testing, and lifestyle modifications in a supportive and empowering environment. Click here to book your free strategy call.
Understanding Hormonal Imbalance
Hormones, integral to myriad bodily functions, act as chemical messengers sent through the bloodstream to tissues and organs. Manufactured by various glands in the endocrine system, these potent chemicals influence everything from growth and metabolism to mood and reproductive health. A delicate balance is crucial for maintaining overall well-being.
When this balance is disrupted—whether due to natural life stages, such as puberty, pregnancy, or menopause, or other factors—your body can experience a range of symptoms. From unexplained weight fluctuations to mood swings, these changes are often indicators that your body’s hormonal equilibrium is off-kilter.
It’s important to recognize these signs early and understand the underlying causes. Hormonal imbalances aren’t just about feeling “out of sorts”; they can significantly impact your long-term health. By being vigilant and proactive, you can work with healthcare providers to address these imbalances, often through lifestyle adjustments, dietary changes, or medical interventions.
Identifying Hormonal Imbalance: What to Look For

Hormonal imbalances can manifest in various ways, often making it challenging to pinpoint the exact cause. Nevertheless, being aware of the common signs can help you recognize potential issues early. One of the primary indicators of a hormonal imbalance is unexplained weight changes. If you find yourself gaining or losing weight without any significant changes to your diet or exercise routine, it might be worth considering if your hormones are playing a role.
Another telltale sign is persistent fatigue. While feeling tired after a long day is normal, constant exhaustion that doesn’t improve with rest could be a red flag. Hormones like cortisol and thyroid hormones significantly influence your energy levels, so imbalances here can leave you feeling drained.
Mood swings and mental health symptoms are also common among those experiencing hormonal imbalances. If you notice sudden shifts in your mood, increased anxiety, or episodes of depression, these might be linked to hormonal fluctuations. Women often report these symptoms during menstrual cycles, pregnancy, and menopause due to changing estrogen and progesterone levels.
Irregular menstrual cycles are another significant indicator. Skipped periods, extremely heavy or irregular cycles, and severe PMS can all point to an imbalance in reproductive hormones such as estrogen and progesterone. Additionally, changes in your skin and hair, like unexpected acne, dry skin, or unusual hair loss, can signify hormonal issues.
Digestive problems like bloating and changes in bowel movements are less commonly known but equally important signs. Hormones such as estrogen and cortisol can impact your digestive health, leading to discomfort and irregularities.
It’s crucial to consult a healthcare professional if you suspect a hormonal imbalance. They can provide appropriate tests and evaluations to get to the root of the problem, ensuring you receive the correct treatment and management strategies.
Common Symptoms of Hormonal Imbalance
Hormonal imbalances can manifest in a variety of ways, often making them challenging to pinpoint. However, certain symptoms are particularly indicative of this issue. Here are some of the most common signs to be aware of:
- Fatigue: Feeling unusually tired despite getting enough sleep can be a red flag. Hormones like cortisol and thyroid hormones play a key role in regulating your energy levels.
- Weight Gain: Unexplained weight gain or difficulty losing weight, especially around the abdomen, is often linked to hormonal imbalances.
- Mood Swings and Depression: Emotional fluctuations or persistent low mood can arise due to imbalances in hormones like estrogen, progesterone, and thyroid hormones.
- Acne: Sudden or severe acne outbreaks, especially in adulthood, can be a sign that your hormones are off balance.
- Digestive Issues: Symptoms such as bloating, diarrhea, or constipation can be tied to an imbalance in hormones that govern digestion.
- Hair Loss: Thinning hair or bald patches can indicate issues with hormones like androgens or thyroid hormones.
- Irregular Sleep Patterns: Struggling with sleep, whether it’s difficulty falling asleep or staying asleep, can be influenced by hormones like melatonin and cortisol.
- Irregular Periods: For women, changes in menstrual cycles, heavy bleeding, or missed periods are often clear signs of hormonal imbalance.
- Night Sweats and Hot Flashes: These are common during perimenopause and menopause but can also signify other hormonal issues.

Recognizing these symptoms early can be crucial for addressing hormonal imbalances effectively. If you experience any of these signs persistently, consulting with a healthcare provider can help you get back on track.
Hormonal Imbalance: Causes and Risk Factors
Hormonal imbalances can strike at any stage in life and are frequently linked to natural hormonal shifts. For instance, puberty, pregnancy, and menopause are notable life stages when hormonal changes are almost inevitable. However, they aren’t the sole culprits. Other causes span a wide range, including chronic stress, autoimmune conditions, injuries to endocrine glands, and the effects of steroids or certain medications.
Chronic stress is a major player in disrupting hormonal equilibrium. When you’re stressed, your body releases cortisol, the stress hormone, which can interfere with the production of other hormones, leading to an imbalance. Certain medications, including steroids and birth control pills, can also have unintended side effects on your hormonal health.
Autoimmune conditions, such as Addison’s disease and thyroid disorders, directly affect hormone-producing glands, making them a significant risk factor. For example, in hypothyroidism, the thyroid gland doesn’t produce enough hormones, leading to various symptoms like fatigue, weight gain, and depression.
Injury or trauma to endocrine glands is another less common but severe cause. These glands, including the pituitary, adrenal, and thyroid glands, are crucial for hormone production. Damage to any of these can result in significant hormonal imbalances.
Lastly, non-physiological factors such as lifestyle choices and environmental exposures also play a role. Poor diet, lack of exercise, significant weight fluctuations, and even exposure to certain chemicals can all impact hormonal levels.
Understanding these causes and risk factors is the first step towards identifying and managing hormonal imbalances. Being aware of what might be affecting your hormones can help you make more informed health choices, bringing you one step closer to balance.
Digestive Problems Linked to Hormonal Imbalance
Hormonal imbalances can affect various bodily functions, and your digestive system is no exception. If you’ve been experiencing persistent digestive issues, such as constipation or diarrhea, it might be time to consider whether your hormones are to blame. But how exactly are these two connected?
Hormones like estrogen and progesterone play significant roles in regulating your gut function. For instance, fluctuations in estrogen levels can slow down or speed up your digestive tract, leading to symptoms like bloating, gas, or changes in stool consistency. Similarly, imbalances in thyroid hormones can also lead to gastrointestinal discomfort, manifesting as either constipation or diarrhea.
Recent research has even suggested a link between hormonal imbalances and irritable bowel syndrome (IBS), especially in people assigned female at birth (AFAB). This connection further underscores the importance of considering hormonal health when diagnosing chronic digestive problems.
If you’re noticing a pattern between your digestive symptoms and phases of your menstrual cycle, stress levels, or weight changes, it may point to a hormonal imbalance. By identifying and addressing these issues, you can take significant steps to improve your digestive health.
Hair Loss and Hormonal Changes
Hair loss can be a distressing experience, and hormones often play a significant role in this issue. Changes in hormone levels, particularly androgens, can trigger hair thinning or significant hair loss. This is especially common during life stages such as menopause, pregnancy, or periods of high stress, where hormonal fluctuations are prominent.
For women, menopause-related hormonal changes can lead to a decrease in estrogen and progesterone levels. These hormones are essential in maintaining hair growth and health. When their levels drop, hair may become thinner, and some women might experience noticeable hair shedding.
On the other hand, an overproduction of androgens, often seen in conditions like polycystic ovary syndrome (PCOS), can lead to hair thinning and even male-pattern baldness in women. It’s not just about losing hair; hormonal imbalances can also cause excessive hair growth in unwanted areas, a condition known as hirsutism.
Identifying hormonal hair loss involves being aware of other associated symptoms of hormonal imbalance, such as menstrual irregularities, weight gain, and skin changes. If you’re noticing changes in your hair alongside these symptoms, it might be time to consult with a healthcare professional for a thorough evaluation.
Understanding the root cause of hormonal hair loss is the first step towards finding an effective treatment plan, which may include lifestyle changes, medication, or various natural remedies designed to rebalance your hormone levels.
Natural Ways to Balance Your Hormones
Seeking natural ways to balance your hormones? You’re not alone. Many individuals turn to holistic and lifestyle approaches before opting for medical intervention. Here’s a guide to help you get started on your journey to hormonal harmony.
Nutrition and Dietary Choices
What you eat plays a vital role in hormone regulation. Prioritize whole, unprocessed foods, and aim for a balanced diet rich in:
- Fiber: Found in fruits, vegetables, and whole grains, fiber aids in detoxifying the body and maintaining steady blood sugar levels.
- Healthy fats: Include sources like avocados, olive oil, and fatty fish. These fats are essential for hormone production.
- Proteins: Lean proteins such as chicken, fish, and plant-based options like beans and lentils provide necessary building blocks for hormone synthesis.
Regular Exercise
Consistent physical activity is a powerhouse for balancing hormones. Not only does it help in maintaining a healthy weight, but it also reduces stress—a common cause of hormonal imbalances. Aim for a mix of aerobic exercises, strength training, and relaxing activities like yoga or tai chi. Remember, consistency is key!
Stress Management
Chronic stress can wreak havoc on your hormones, leading to issues like adrenal fatigue and thyroid disorders. Incorporating stress-reducing practices such as meditation, deep-breathing exercises, or even hobbies you enjoy can foster a more balanced hormonal environment.
Adequate Sleep
Quality sleep is non-negotiable for hormonal health. Aim for 7-9 hours of restful sleep per night. This will aid in the regulation of cortisol levels and ensure your body has time to repair and produce hormones.
Limit Toxins and Endocrine Disruptors
Exposure to toxins found in some household cleaners, plastics, and even cosmetics can affect your hormonal balance. Opt for natural cleaning products, avoid plastic containers, and choose organic produce when possible to reduce exposure to harmful chemicals.
Hydration
Staying adequately hydrated is often overlooked but is crucial for hormone transport throughout the body. Aim for at least 8 glasses of water a day, and consider herbal teas like chamomile or green tea, which offer additional antioxidant benefits.
Balancing your hormones naturally involves a holistic approach. By incorporating these lifestyle changes, you can start to feel more balanced and in control of your hormone health. Remember, it’s about consistency and creating habits that support your overall well-being.
Hormone Testing: What You Need to Know
When it comes to diagnosing hormonal imbalances, pinpointing the exact issue can often feel like solving a mystery. Doctors typically begin by documenting your specific symptoms and health history. This preliminary information is critical; it guides what types of hormone tests might be necessary.
Blood tests are a common method for measuring hormone levels. These tests can detect hormones circulating in the bloodstream, providing essential data about what’s going on internally. Hormones such as estrogen, testosterone, cortisol, and thyroid hormones are often part of this testing process.
While blood tests are a primary tool, they aren’t the only option. At-home tests have become increasingly popular, providing convenience and privacy. These tests may involve saliva, blood, or urine samples. However, it’s essential to follow up any at-home test results with your healthcare provider to ensure accuracy and appropriate treatment.
For women, timing can be crucial in hormone testing. Specific hormone levels fluctuate throughout the menstrual cycle. Therefore, your doctor may recommend testing on particular days to get the most accurate readings. This is particularly relevant for hormones like progesterone and estrogen.
Utilizing functional testing such as the DUTCH hormone test, GIMAP stool test, and HTMA hair mineral test are just some of the tests you can utilize to get more answers around your hormone health. In our practice, we use all of these tests and more to help you uncover the root cause of your hormone and fertility challenges.
If you’d like more support with your hormone health, book a strategy call right here.
Throughout this article, we’ve explored the intricacies of hormonal imbalances, addressing their causes, symptoms, and natural remedies. By understanding the root factors and signs of hormonal disorders, you can take proactive steps towards managing your health more effectively. Recognizing digestive issues, hair loss, or sudden mood changes can be critical indicators to seek professional advice.
In conclusion, maintaining balanced hormones is key to overall well-being. It’s important to listen to your body and identify any unusual symptoms early. With proper dietary choices, regular exercise, stress management, and adequate sleep, you can naturally support your hormonal health. Remember, professional guidance is invaluable – don’t hesitate to reach out to healthcare experts to help navigate your hormonal health journey.
Introduction to Recurrent Pregnancy Loss
Facing recurrent pregnancy loss (RPL) can be both emotionally and physically draining. Defined by the American Society for Reproductive Medicine (ASRM) as two or more consecutive pregnancy losses, RPL affects approximately 1-2% of couples trying to conceive. Traditionally, it was defined as three or more losses, but recent guidelines from the European Society of Human Reproduction and Embryology (ESHRE) have adopted the more inclusive definition.
Understanding the root causes of RPL is essential for finding effective treatments and support. The journey often involves a multitude of factors, from genetic anomalies to hormonal imbalances, and even infections. Although the causes can be complex, advancements in research and technology offer hope for affected couples.
Our goal here is to explore various underlying reasons behind RPL, the diagnostic tests available, and the emerging treatments promising to make an impact. Whether you’re experiencing this challenging condition or supporting someone who is, this guide aims to provide the information needed for a proactive approach to managing recurrent pregnancy loss.

Genetic Factors Behind Recurrent Pregnancy Loss
When it comes to recurrent pregnancy loss (RPL), genetics play a pivotal role. Chromosomal anomalies, whether in the parents or the embryo, contribute significantly to this heart-wrenching condition. A karyotype analysis, which examines the number and structure of chromosomes, is often recommended for both partners to identify any genetic irregularities. Coupled with other diagnostic tests, this can uncover potential genetic causes behind RPL.
Most pregnancy losses occur due to random chromosomal abnormalities, such as aneuploidy, which is the presence of an abnormal number of chromosomes in a cell. These anomalies often happen spontaneously and are not typically inherited. However, certain genetic defects in either parent can increase the risk of such random events. If a parent is a carrier of a balanced translocation, for instance, it can lead to unbalanced translocations in the embryo, resulting in miscarriage.
An emerging field of study is the role of single nucleotide polymorphisms (SNPs) in pregnancy loss. SNPs are variations in a single nucleotide that occur at a specific position in the genome. While the impact of SNPs is still under investigation, some have been linked to reproductive issues, providing another layer of complexity to the genetic factors involved in RPL.
Knowing these factors allows for tailored approaches when considering future pregnancies. Genetic counseling is often recommended to help couples understand their risk and explore reproductive options. For some, preimplantation genetic testing (PGT) during in vitro fertilization (IVF) might be a viable option, as it allows for the selection of embryos without specific genetic anomalies.
Understanding the genetic basis of recurrent pregnancy loss is fundamental. By addressing these factors, couples can be better prepared and supported in their journey toward a successful pregnancy.
Hormonal Imbalances: A Hidden Culprit
Hormonal imbalances are often overlooked yet significant contributors to recurrent pregnancy loss (RPL). Common endocrine disorders, such as thyroid disease and diabetes, can profoundly impact pregnancy viability. For instance, hypothyroidism, a condition where the thyroid gland does not produce sufficient hormones, can disrupt the delicate hormonal balance required for a successful pregnancy. Similarly, uncontrolled diabetes can lead to poor blood sugar control, which adversely affects fetal development.
Another frequent hormonal imbalance involves the levels of progesterone, a hormone crucial for maintaining the uterine lining during pregnancy. Insufficient progesterone can result in the uterine lining shedding prematurely, leading to miscarriage. Hormonal fluctuations brought about by polycystic ovary syndrome (PCOS) can also elevate the risk of pregnancy complications, as the condition often results in irregular ovulation and associated hormonal imbalances.
Addressing these hidden culprits requires a proactive approach. Comprehensive hormonal screenings and timely interventions can help regulate these imbalances. Potential treatments might include thyroid hormone replacement therapy, insulin management for diabetes, and progesterone supplementation. By stabilizing these hormonal levels, it’s possible to create a more conducive environment for pregnancy, substantially reducing the risk of RPL.
It’s essential to discuss any symptoms or concerns with your healthcare provider. Identifying and managing hormonal issues early can offer hope and improve outcomes for those affected by recurrent pregnancy loss.
Genetic Factors Behind Recurrent Pregnancy Loss
When delving into the genetic factors behind recurrent pregnancy loss (RPL), it becomes evident that variations in chromosomes are often to blame. Around half of first-trimester miscarriages are linked to chromosomal abnormalities, such as aneuploidy – the gain or loss of one or more chromosomes. These abnormalities can result in conditions like Turner syndrome and Down syndrome, leading to pregnancy loss.
Additionally, structural chromosomal rearrangements, including translocations and inversions, can also contribute to RPL. In such cases, the parents may carry balanced rearrangements that go unnoticed until they attempt to conceive, only to result in recurrent miscarriages. Karyotype analysis of both partners can help in detecting these chromosomal issues, allowing for an informed approach to treatment or reproductive alternatives like IVF with preimplantation genetic testing.
The genetic architecture of sporadic versus recurrent miscarriage also shows marked differences. While a single miscarriage might be attributed to sporadic genetic mutations, recurrent miscarriages often indicate a deeper genetic predisposition. Recent research involving genome-wide scans in sibling pairs with idiopathic recurrent miscarriage has revealed genetic linkages, suggesting a hereditary component that warrants further investigation.
Moreover, advanced maternal age is a significant factor contributing to genetic anomalies. Women over 35 years old face a higher risk of chromosomal aberrations in their ova, increasing the likelihood of recurrent pregnancy loss. With age, the quality and genetic integrity of a woman’s eggs decline, resulting in a higher probability of abnormal embryonic development.
Ultimately, understanding the genetic factors involved in RPL is crucial for developing targeted interventions. While genetic counseling and testing are fundamental tools, ongoing research and emerging technologies are continually improving our ability to diagnose and manage these complex genetic issues.
The Role of Infections in Recurrent Pregnancy Loss
While the role of infection in first-trimester recurrent pregnancy loss (RPL) remains somewhat ambiguous, it’s a factor that cannot be entirely ruled out. Infectious agents might contribute to pregnancy loss if they establish a persistent presence in the reproductive tract. Some studies suggest infections, particularly chronic or undetected, could disrupt the delicate balance necessary for a successful pregnancy.
Bacterial vaginosis, for example, has been associated with adverse pregnancy outcomes, including RPL. Similarly, certain viral infections like cytomegalovirus (CMV) and herpes simplex virus (HSV) have been explored in connection with pregnancy complications. However, the exact mechanisms by which these infections might lead to recurrent losses are not fully understood and require more in-depth research.
Furthermore, infections that trigger an inflammatory response can be particularly problematic. Inflammation can impair implantation or placental development, both crucial for sustaining a pregnancy. Therefore, a thorough evaluation for infections may be a necessary step in identifying the root causes of unexplained RPL.
At times, treating an underlying infection can improve pregnancy outcomes. For instance, antibiotics may be prescribed if a bacterial infection is detected. However, the decision to treat depends on a comprehensive diagnosis and understanding of the specific infections involved.
In conclusion, while infections are a potential factor in RPL, the challenge remains in their identification and the understanding of their exact impact. Future research focusing on the relationship between infectious agents and pregnancy loss could offer deeper insights and pave the way for more effective management strategies.
Autoimmune Disorders and Pregnancy Loss
Autoimmune disorders play a critical role in recurrent pregnancy loss (RPL). These disorders occur when the body’s immune system mistakenly attacks its own tissues. In the case of pregnancy, sometimes the immune system may target the placenta or developing embryo, leading to complications.
A prominent example of this is Antiphospholipid Syndrome (APS). This condition is characterized by the presence of antiphospholipid antibodies, such as anticardiolipin and lupus anticoagulant, which can interfere with normal blood clotting and contribute to pregnancy loss. Early miscarriage, stillbirth, and other pregnancy complications are often linked to APS. If you have a history of autoimmune disorders, discussing APS testing with your healthcare provider is crucial for a thorough evaluation.
Another autoimmune factor to consider is the role of anti-inflammatory cytokines. These specialized proteins are part of the body’s immune response and can be produced by placental and decidual tissues. However, an overproduction may result in inflammation, disrupting the environment necessary for a successful pregnancy.
Research and updated 2023 ESHRE guidelines have pointed out the importance of scrutinizing autoimmune factors in recurrent pregnancy loss. Diagnostic tests often focus on identifying these antibodies and assessing immune function. It’s worth noting that early and accurate diagnosis can significantly improve management and treatment options, increasing the chances of a successful pregnancy.
Understanding how autoimmune disorders contribute to recurrent pregnancy loss underscores the importance of a holistic approach to diagnosis and treatment. By addressing these underlying issues, healthcare providers can offer more personalized and effective care plans, ultimately supporting a healthier pregnancy journey for those affected by RPL.
Diagnostic Tests for Uncovering Root Causes

Getting to the bottom of recurrent pregnancy loss involves a comprehensive and often multifaceted approach. The first step typically involves a detailed medical history and physical examination. This initial evaluation can offer vital clues and help in tailoring further testing.
Beyond the basics, specialized tests are essential for identifying the underlying causes. Blood tests can reveal hormonal imbalances by measuring levels of thyroid-stimulating hormone (TSH) and prolactin, which play critical roles in maintaining a healthy pregnancy. Similarly, antiphospholipid antibody (APA) and thrombophilia testing can detect autoimmune disorders that might contribute to pregnancy loss.
Genetic testing is another crucial component. Karyotype analysis of both partners can identify chromosomal abnormalities that might be a significant cause of recurrent pregnancy loss. In some cases, cytogenetic testing of the pregnancy tissue itself is performed to look for abnormalities in the fetus.
Some studies suggest testing for Factor V Leiden (FVL) mutations, especially in cases of unexplained or idiopathic early recurrent pregnancy loss. Though not always conclusive, such tests can provide invaluable information for managing the condition.
Imaging studies also play a vital role. Ultrasound (US) examinations or histopathologic evaluations of the uterine cavity can identify structural abnormalities like fibroids or a septate uterus, which might hinder a successful pregnancy.
Ultimately, the goal is to identify modifiable etiological and risk factors for effective treatment. By combining detailed medical history, specialized blood tests, genetic testing, and imaging studies, you and your healthcare provider can develop a personalized strategy aimed at overcoming recurrent pregnancy loss.
| Study | Year | Factor Investigated | Impact on Recurrent Pregnancy Loss |
| Evans, J. et al. | 2018 | Genetic Factors | Significant |
| Johnson, R. et al. | 2017 | Hormonal Imbalances | Moderate to High |
| Smith, A. et al. | 2019 | Infections | Low to Moderate |
| Lee, C. et al. | 2020 | Autoimmune Disorders | High |
Identifying the Root Causes of Recurrent Pregnancy Loss
When it comes to recurrent pregnancy loss (RPL), identifying the root causes is crucial. The complexity of RPL means that it often results from a multifactorial interplay of genetic, hormonal, anatomical, and immunological factors. Each potential cause warrants careful investigation and testing to develop an effective management plan.
Genetic Factors: Chromosomal abnormalities are a common cause of RPL. A detailed medical history and karyotype analysis of both partners can reveal genetic irregularities. Advanced techniques like a 24-chromosome microarray analysis of miscarriage tissue have shown to determine a probable or definite cause in over 90% of cases.
Hormonal Imbalances: Hormonal issues, such as thyroid disorders, polycystic ovary syndrome (PCOS), or luteal phase insufficiency, can significantly impact pregnancy viability. Blood tests and hormonal profiling help in detecting these imbalances, allowing for targeted treatments.
Anatomical Abnormalities: Uterine anomalies like septate uterus, fibroids, or adhesions can prevent the proper implantation and growth of the embryo. Imaging techniques, such as hysterosonography or MRI, can identify these structural issues. Surgical interventions often correct them, improving pregnancy outcomes.
Immunological Factors: Autoimmune disorders, where the body’s immune system mistakenly attacks its own tissues, can also play a role. Conditions like antiphospholipid syndrome (APS) need specific blood tests and expert evaluation for a definitive diagnosis, followed by immune-modulating therapies.
Infections: Certain infections can disrupt the delicate environment of the uterus, leading to pregnancy loss. Screening for infections and appropriate treatments are vital, especially if there’s a history suggestive of infectious agents.
Understanding these potential causes, through a combination of detailed medical history, meticulous physical examination, and a spectrum of diagnostic tests, is key in offering hope and tailored treatments to women struggling with recurrent pregnancy loss.
Future Research and Emerging Treatments
As we look ahead, the field of recurrent pregnancy loss (RPL) is evolving with promising avenues of research and innovative treatments. One particularly exciting area is the use of next-generation sequencing (NGS). This technology allows for an in-depth examination of genetic factors that may contribute to RPL, offering more personalized and targeted approaches to treatment. By pinpointing specific genetic anomalies, clinicians can tailor interventions to the individual needs of each couple, potentially improving outcomes significantly. Additionally, there’s a growing recognition of the importance of addressing the psychosocial needs of couples dealing with RPL. Future studies and treatment plans are increasingly incorporating mental health support as a crucial component. This holistic approach not only aims to improve emotional well-being but also to provide comprehensive care that addresses both physical and psychological factors of pregnancy loss.
While various treatments are currently available, there is no one-size-fits-all solution. This is where more extensive randomized controlled trials (RCTs) come into play. There is a pressing need for larger and more rigorous trials, ideally conducted across multiple centers, to evaluate the efficacy of different surgical procedures and medical treatments. Such research efforts would provide clearer guidelines and more effective management strategies for RPL.
Current meta-analyses often consider a diverse array of patient populations and treatment methodologies, resulting in inconsistent recommendations. Therefore, future analyses must focus on more homogenous patient groups to derive more applicable and precise conclusions. By refining the subsets of patients studied, we can ensure that the resulting data is both relevant and practical for specific demographics.
Another crucial aspect is the development of improved prognostic tools. These tools aim to predict the likelihood of pregnancy loss recurrence, empowering healthcare providers to devise more effective, customized treatment plans. This predictive capability is vital in managing expectations and creating proactive medical strategies for couples at risk.
Ultimately, the goal is to enhance our understanding of the modifiable etiological and risk factors associated with RPL. By identifying and addressing these factors, treatment strategies can become more effective, leading to better outcomes for those affected. As research progresses, the hope is that emerging treatments and interventions will offer new hope and possibilities for couples experiencing recurrent pregnancy loss.
Getting Support
If you’re looking for more support on your fertility journey, utilizing functional nutrition, you can apply to work with our team of dedicated fertility dietitians here.
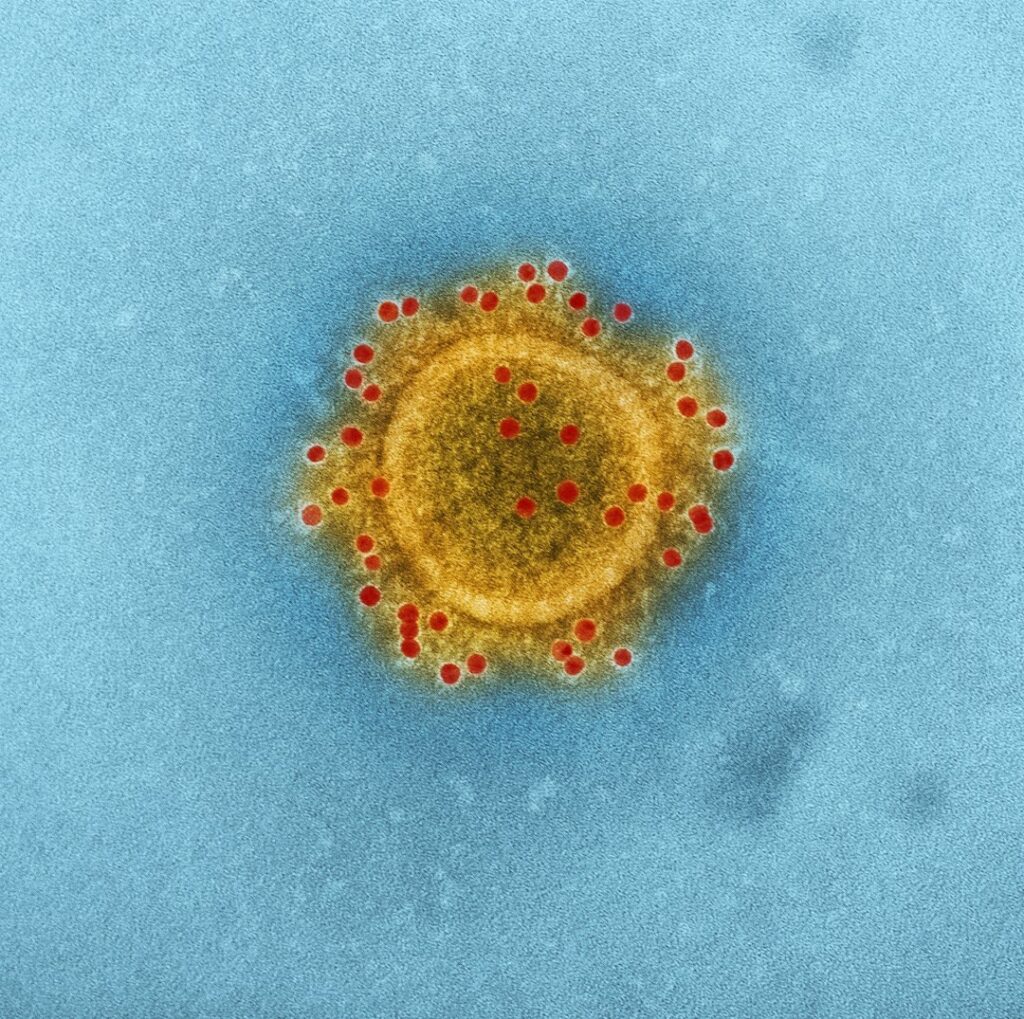
The Science Between Antioxidants and Reproductive Health
Antioxidants are molecules that neutralize harmful free radicals in your body. Free radicals are unstable atoms that can damage cells, leading to oxidative stress. This oxidative stress is believed to impact health negatively, including your reproductive health. Scientific studies have increasingly explored the role of antioxidants in fertility, with many findings suggesting a positive impact.
Antioxidants are known to combat oxidative stress, which can damage cells, including sperm and egg cells. By neutralizing free radicals, antioxidants help maintain cellular integrity and function, which is crucial for reproductive health. One notable study published in the journal ‘Fertility and Sterility’ found that men who took antioxidant supplements experienced improvements in sperm quality, including increased motility and reduced DNA fragmentation. This suggests that antioxidants can enhance male fertility by protecting sperm from oxidative damage.
The relationship between antioxidants and reproductive health is rooted in the protective role antioxidants play. By neutralizing free radicals, antioxidants help maintain the integrity of your cells, including sperm and egg cells. Reducing oxidative stress can result in better quality eggs, enhanced sperm function, and an overall improved environment for conception.
Consider antioxidants as a form of cellular defense. When your body has an adequate supply, it can combat oxidative damage more effectively. This is particularly beneficial for your reproductive system, where cell quality is crucial for successful fertilization and a healthy pregnancy.
Research supports this connection. Studies have shown that higher serum concentrations of antioxidants correlate with better reproductive outcomes. In women, antioxidants support healthy steroidogenesis, the process by which sex steroids are produced, essential for ovulation and menstrual cycle regulation. In men, antioxidants improve sperm quality, motility, and overall fertility.
Moreover, specific antioxidants have been identified as instrumental in fertility. Vitamins C and E, beta-carotene, and selenium are just a few that have been extensively studied. They help in reducing oxidative stress and improving the health of reproductive cells. Knowing this, incorporating antioxidant-rich foods into your daily diet can be a strategic move for enhancing your reproductive health.
How Do Antioxidants Improve Fertility?

Antioxidants work their magic by directly combating oxidative stress (OS), a condition characterized by an imbalance between free radicals and antioxidants in your body. Free radicals are unstable molecules that can damage cells, including the delicate cells involved in reproduction. By neutralizing these free radicals, antioxidants protect your eggs and sperm from oxidative damage.
When oxidative stress is reduced, the quality of both eggs and sperm can improve significantly. For women, this means healthier eggs that are more likely to result in successful fertilization, embryo quality, and ultimately, a viable pregnancy. Improved egg quality is especially critical for those dealing with age-related fertility challenges or conditions like polycystic ovary syndrome (PCOS).
On the male side, antioxidants play an equally crucial role. They help enhance sperm quality by improving motility, morphology, and overall DNA integrity. Healthier sperm increases the chances of successful fertilization and reduces the risk of miscarriage and genetic abnormalities.
Additionally, antioxidants can support the overall environment of your reproductive system, contributing to better ovarian function and uterine health. This balanced environment is crucial for conception and maintaining a healthy pregnancy. Thus, whether you’re trying to conceive naturally or with the assistance of IVF or ICSI, incorporating antioxidants into your routine can be a powerful ally in your fertility journey.
What Causes Oxidative Stress?
Oxidative stress is a condition that arises when there’s an imbalance between free radicals, specifically reactive oxygen species (ROS), and the body’s ability to neutralize them with antioxidants. It’s like a tug-of-war happening in your cells, and when the scales tip in favor of ROS, the result is oxidative damage.
This oxidative damage can affect various parts of your body, but when it comes to fertility, both male and female reproductive health can take a hit. Let’s dive into some common causes. First off, poor lifestyle choices such as a lack of regular exercise, overeating, or a diet rich in sugars and unhealthy fats are significant contributors. These habits increase ROS levels while depleting your antioxidant reserves, creating a fertile ground for oxidative stress.
Environmental factors also play a crucial role. Exposure to pollutants, toxins, and radiation can ramp up ROS production. Then there’s the unavoidable factor of aging. As we age, our body’s cellular energy production decreases, and we’re naturally more prone to oxidative stress.
Not to be overlooked, physical and emotional stress can trigger oxidative stress as well. Chronic stress encourages the production of ROS, leading to cellular damage and decreasing your body’s capacity to fend off these unwelcome molecules.
Understanding these causes helps you take proactive steps to mitigate oxidative stress, ultimately creating a better environment for reproductive health. Now, let’s explore how antioxidants step in to level the playing field.
Key Antioxidants That Boost Fertility

Okay, now that we know that we want LESS oxidative stress and MORE antioxidants – how do we actually do that?
First, focus on incorporating antioxidant-rich foods into your daily diet. These foods are not only delicious but can also help boost your fertility. Think colorful fruits and vegetables, nuts, seeds, and whole grains. Berries, spinach, and dark chocolate are all excellent choices packed with antioxidants to help fight oxidative stress.
In addition to a diverse diet, consider omega-3 fatty acids, which have been shown to reduce prostanoids and increase antioxidant effects. You can find these in fatty fish like salmon, as well as in flaxseeds and walnuts. Not only do these foods help balance your antioxidant levels, but they also add variety and flavor to your meals.
Don’t forget about lifestyle factors! Regular physical activity can enhance your body’s ability to manage oxidative stress. Likewise, stress-reduction techniques such as meditation, yoga, or even simple daily walks can have a positive impact on your oxidative balance.
Finally, avoid exposure to toxins as much as possible. This includes reducing your intake of processed foods, quitting smoking, limiting alcohol consumption, and avoiding areas with high pollution. These changes might seem challenging, but they’re essential steps toward decreasing oxidative stress and creating a fertile environment. Antioxidants help combat oxidative stress, which can damage reproductive cells.
By taking these steps, you’ll be on your way to a healthier, more balanced body, primed for fertility. Remember, while it might take some time to see the effects, every small change counts.
Top Antioxidant-Rich Foods for Fertility
When it comes to enhancing your fertility through diet, loading up on antioxidant-rich foods is crucial. These foods combat oxidative stress, protect your eggs and sperm, and provide a fertile foundation for conception. Eating a diverse range of fruits and vegetables is an excellent way to ensure you’re getting the antioxidants you need.
Here are some top choices to consider:
- Berries: Blueberries, strawberries, raspberries, and blackberries are bursting with antioxidants and vitamins that support reproductive health.
- Leafy green vegetables: Spinach, kale, and Swiss chard are not only packed with antioxidants but also loaded with folate, which is essential for healthy fetal development.
- Citrus fruits: Oranges, grapefruits, lemons, and limes are excellent sources of vitamin C, a powerful antioxidant that can enhance the quality of both eggs and sperm.
- Nuts and seeds: Almonds, walnuts, and sunflower seeds are high in vitamin E, which helps protect sperm and egg DNA from damage.
- Colorful vegetables: Vegetables like carrots, sweet potatoes, and bell peppers contain beta-carotene, an antioxidant that converts to vitamin A in the body, supporting hormonal health.
- Tomatoes: Rich in lycopene, tomatoes can improve sperm quality and reduce the risk of oxidative stress.
Incorporating these foods into your daily diet can create a positive impact on your fertility. Remember, balance and variety are key. Aim to fill your plate with a rainbow of colors to maximize the benefits of different antioxidants.
| Antioxidant | Natural Sources | Impact on Fertility |
| Vitamin C | Citrus fruits, strawberries, bell peppers | Improves sperm quality, reduces oxidative DNA damage |
| Vitamin E | Nuts, seeds, leafy greens | Enhances endometrial lining, crucial for implantation |
| Coenzyme Q10 | Meat, fish, whole grains | Improves ovarian response, boosts egg quality |
| Selenium | Brazil nuts, seafood, eggs | Protects sperm from oxidative damage, supports reproductive health |
| Zinc | Oysters, beef, spinach | Essential for hormone regulation, improves sperm formation |
Incorporating antioxidant-rich foods into your diet can significantly enhance both male and female fertility by reducing oxidative stress and improving reproductive health. These vital nutrients work to protect and improve egg and sperm quality, support hormone regulation, and create a more favorable environment for conception. By understanding and utilizing the power of antioxidants, you’re taking a proactive step towards boosting your fertility and optimizing your chances of a successful pregnancy.
Looking for More Support on Your Fertility Journey?
You can apply for a free strategy call to see which program would be the best for you. Our team of dedicated fertility practitioners will help you gain answers, clarity, and a roadmap to naturally enhance your fertility using science-backed methods and a food as medicine approach.
The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook