Resources
Style
Planning
View All
THE blog
By: Josie Mangano
Reviewed By: Anabelle Clebaner MS, RDN
It’s commonplace for women to are trying to conceive to track their menstrual phases. However,
did you know that whether or not you’re trying to conceive, tracking the phases of your
menstrual cycle can be a valuable tool for assessing overall health and wellbeing? If you have
PCOS or are experiencing symptoms related to hormone imbalance, fertility awareness may
help you understand the cues your body is giving you in order to address the root causes.
Irregular menstrual cycles are linked to nutritional deficiencies, energy deficits, hormonal acne,
and even loss of bone density in the long-term. Put simply, your hormone health is important
even before you are trying to conceive.
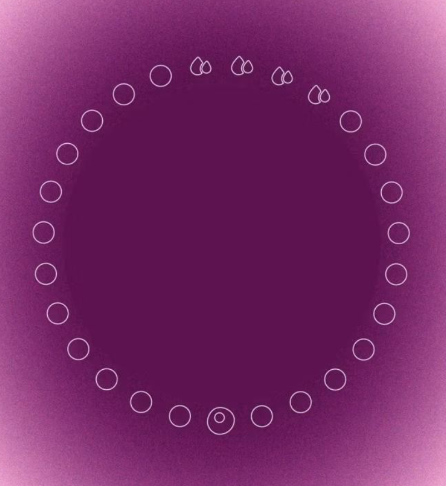
What is Fertility Awareness?
Fertility awareness — is a set of practices that are used to determine the fertile and infertile
phases of your menstrual cycle.
The techniques used to track menstruation and ovulation are known as Fertility Awareness
Methods (FAMs). But first, let’s review what you should know about the menstrual cycle, the
fertile window, and what the patterns of a normal cycle look like.
What You Need to Know About the Menstrual Cycle
A normal menstrual cycle lasts anywhere between 24-35 days. The first day of your period
(when flow begins) is always considered day 1 of your cycle. Normal menstruation lasts
between 3-7 days.
In the days following menstruation, your ovaries release an egg into the fallopian tubes — this
process is called ovulation. This egg stays in your fallopian tubes and, if not fertilized by a
sperm, will dissolve after 12-24 hours. Contrary to the myth that ovulation occurs 14 days after
your period starts, ovulation typically happens between days 10-23, depending on the length of
your cycle. It is essential to note that sperm can survive in the female reproductive tract for up to
5 days. Therefore, your fertile window is classified as the 5 days before ovulation, the day of
ovulation, and the following day (7 days total).
During the fertile window, the sperm present in the female reproductive tract may fertilize an egg
and implant itself in the uterine lining, thus marking the beginning of pregnancy. If the egg is not
fertilized and the egg is reabsorbed, hormones drop, and menstruation occurs, marking the
beginning of a new cycle. After the fertile window passes, pregnancy is not possible because
the egg is no longer present for fertilization. The days after ovulation and before menstruation
are referred to as the post-ovulatory phase.
With that covered, we can dive into the science-backed tools we use for fertility awareness cycle
tracking.

The 3 main fertile signs to pay attention to are:
1. Cervical mucus
2. Basal body temperature (BBT)
3. Cervical position
Let’s review each of these signs more closely and learn how they may be related to underlying
causes such as hormone imbalances, nutrient deficiencies, and/or underlying health conditions.
Cervical Mucus
The presence of cervical mucus (CM) is indicative of your fertile window. CM plays an essential
role in natural conception by matching the pH of sperm, creating the perfect environment for it to
stay alive for up to 5 days in the otherwise hostile female reproductive tract.
There are two kinds of cervical mucus that are often referred to when it comes to reproductive
health. The first is “peak mucus” which is an optimal environment for sperm and is also an
indicator of a healthy cycle when present in the fertile window. Peak mucus is clear, stretchy,
and is comparable to egg whites. There is also “non-peak mucus” which is cloudy, white, and similar to creamy hand lotion. Non-peak mucus is not as optimal because it is hostile to sperm.
It is usually present shortly after menstruation and later in the menstrual cycle (luteal phase).
However, it is important to note that all mucus is fertile in the pre-ovulatory phase! Pregnancy
can occur in the presence of either kinds of CM in the fertile window

If your experience with CM differs, there are some red flags we can look for to assess
underlying hormonal imbalances and/or health conditions.
Cervical Mucus Red Flags
Limited or no mucus — can indicate an issue with hormone production, the cervix, or other
related issues including HPV, cervical dysplasia, or use of medications like hormonal birth
control, fertility drugs, or antihistamines. Can indicate inadequate nutrient intake of cholesterol
(to support estrogen and progesterone production), vitamin A, and B vitamins (folate). Can
indicate endocrine issues such as thyroid disorder, HPA axis dysregulation, hypothalamic
amenorrhea, etc.
Continuous mucus — can indicate an issue in the cervix, or presence of infection,
inflammation, or hormone imbalance.
Continuous creamy/lotiony (non-peak) mucus — may indicate an overgrowth of
yeast/bacteria. During the luteal phase, low progesterone production may contribute to
continuous non-peak mucus.
Continuous clear/stretchy (peak) mucus — seen in women with PCOS and/or women
experiencing food sensitivities, IBS, and other gut-related issues in the pre-ovulatory phase.
Yellow-tinged mucus – can be indicative of infection.
Basal Body Temperature (BBT)
Basal Body Temperature can be measured by taking your temperature first thing in the morning,
before getting. It is important that you do this immediately after waking up for an accurate
reading, before eating or drinking.
Tracking these temperatures provides us with the information we need to confirm when
ovulation occurs, but keep in mind that there is no way to predict when ovulation will occur due
to extraneous factors like travel and stress which may delay ovulation. You can keep track of
your BBTs by either logging them manually on a BBT chart or by using a fertility tracking app.
Normal pre-ovulatory temperatures should consistently be above 97.5° F ranging up to about
98.2 °F. Normal post-ovulatory temperatures should be higher than the pre-ovulatory range with
at least one temperature higher than 98.6 °F. Temperatures that fall consistently lower than this
range indicate potential health issues and nutrient deficiencies.
What are Some Possible Causes of Low Basal Body Temperatures?
Possible causes of low BBT include nutrient deficiencies of nutrients involved in thyroid function
such as zinc, iron, selenium, and iodine. Iron deficiency may also contribute to low BBTs since
iron is highly involved in body temperature regulation. Zinc and iron supplementation have
independently been shown to improve thyroid hormone levels and thus increase BBTs in
deficient women.
Low BBTs may also result from inadequate calorie consumption from skipping meals or failing
to consume enough calories to offset exercise levels. Poor sleep may also contribute to low
BBTs by offsetting natural circadian rhythms. Finally, thyroid disorders such as hypothyroidism
and Hashimoto’s thyroiditis play a role in lowering BBTs.
Cervical Position
The final indicator of fertility is cervical position, which changes throughout the menstrual cycle.
By regularly checking cervical position we can better understand our bodies through common
patterns that we notice throughout our cycles.
But what is the cervix and how can we use it to track our cycles?
The cervix is the small, muscular organ that connects the vagina to the uterus. It’s a round,
prominent structure with a hole in the middle that’s roughly an inch in diameter. It produces
cervical mucus, expels menstrual flow, allows sperm to pass through during ovulation, and acts
as a barrier against infections.
During ovulation, high estrogen levels cause the cervix to rise closer to the top of the vagina.
The cervix often feels softer during the fertile window. As mentioned previously, the cervix is
responsible for producing peak CM during this time.
After ovulation (luteal phase), the position of the cervix lowers to prepare for menstruation. This
cervix tends to lower or “drop” on average a week to 10 days before menstruation begins.
During menstruation, the cervix remains low and opens slightly to release the menstrual blood
flow. The cervix feels firm to the touch during this time and will continue to feel this way until
after your period ends.
In early pregnancy, the position of this cervix is high in the vagina, similar to its position during
ovulation. The cervix is known to feel soft during this time, however it is important to use a
pregnancy test to confirm pregnancy as cervical position is not a guarantee in confirming early
pregnancy.
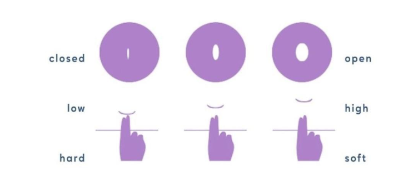
For more information on how to check your cervical position, click here.
Now that we’ve laid the groundwork of cycle tracking, let’s discuss some specific nutrients and
how they uniquely benefit cervical health!
Key Nutrients to Support Cervical Health
1. Folate — has been shown to reverse abnormal (precancerous) cervical cells and reverse
cervical dysplasia. Folate plays a key role in supporting healthy cell division, most notably
during early pregnancy in the formation of the spinal cord.
2. Vitamin A (retinol) — has been shown to reverse abnormal cervical cells when applied
topically to the cervix. Vitamin A is critical for fertility and plays a role in preparing the uterine
lining for implantation. Pregnant women should avoid all forms of vitamin A supplementation.
Dark leafy greens, red/orange vegetables, beef, eggs, and dairy products are rich in vitamin A.
3. Indole-3-Carbinol – has been shown to reverse abnormal cervical cells in clinical trials.
I3C plays a role in modulating estrogen metabolism and is a compound found in cruciferous
vegetables like broccoli, brussels sprouts, kale, and cauliflower

There you have it — the 3 main fertile signs to pay attention to and related cues that can give us
powerful insights into our hormonal and reproductive health. If you feel passionate about using
fertility awareness as a guide to managing hormonal imbalances, managing PCOS, or preparing
your body for the healthiest pregnancy possible, consider reaching out to our team at Wellspring
Nutrition for 1:1 functional nutrition counseling and a personalized plan to achieve your unique
health goals.
References
Hendrickson-Jack L. Women’s Health Nutrition Academy (WHNA). “Unlocking the Secrets of the
Menstrual Cycle: How Fertility Awareness Cycle Tracking Can Help Your Nutrition Practice”.
Sumner C. Cervix positions: What they mean & how to check them. Natural Cycles. Published
June 28, 2022. https://www.naturalcycles.com/cyclematters/cervix-positions-explained
If you’ve ever been told “everything looks normal”-yet nothing feels normal at all- you know how deeply frustrating those words can be.
You watch friends, coworkers, even strangers announce pregnancies that seemed to happen effortlessly. Meanwhile, you’re tracking, testing, timing and doing everything under the sun… and still, nothing. It’s exhausting. It’s isolating. It can make you feel like you’re somehow missing something obvious.
You’re not.
So many couples reach this same breaking point after hearing that familiar line, “everything looks fine.” It can feel like the end of the road- like the doctors have checked their boxes and moved on, even though your gut tells you something isn’t adding up. Because if everything were truly fine, this wouldn’t feel so hard.
Hormone testing can be incredibly helpful. It gives us a valuable snapshot of what’s happening beneath the surface, at the microscopic level. But here’s the truth, hormones don’t tell the whole story.
Fertility isn’t controlled by a single switch or dictated by hormones alone. It’s a complex, multi-factorial system influenced by far more than any one lab result can capture. When something feels off, it’s worth looking deeper- because “normal” doesn’t always mean optimal, and it certainly doesn’t mean your experience isn’t valid.
What does “normal” hormone blood work actually mean?
When it comes to fertility, hormones are the behind-the-scenes directors calling the shots. But which hormones actually matter- and when should they be tested? Let’s break it down.
Key players we look at for fertility include follicle-stimulating hormone (FSH), luteinizing hormone
(LH), estradiol (E2), anti-Müllerian hormone (AMH), and Progesterone. Together, these hormones
help paint a clear picture of ovarian reserve and overall reproductive function. Most of these labs are checked on day 3 of your menstrual cycle, and that timing isn’t random. Day 3 of your cycle is when many of these hormones are at their lowest, or most baseline, levels. Testing consistently on this day allows us to compare apples to apples each month. Without that consistency, hormone levels can jump all over the chart, making us compare apples to oranges

The “normal” reference ranges you see on lab reports aren’t always the same as optimal ranges for
fertility. Those reference ranges are designed to catch diseases or major deficiencies -not to tell us
whether your body is operating at peak reproductive potential. So yes, you can fall within the “normal” range and still have room for improvement when it comes to fertility.
In short: the right hormones, the right timing, and the right interpretation make all the difference when it comes to understanding your fertility.
Why can Standard labs miss fertility root causes?
As mentioned earlier, the cornerstone hormones assessed in routine fertility testing include
follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), anti-Müllerian
hormone (AMH), and Progesterone. These labs are undeniably important and offer valuable insight into reproductive function. But fertility is far more nuanced than a handful of numbers on a lab report- and there are critical factors these values simply can’t capture.
Blood sugar regulation plays a foundational role in fertility. When blood sugar is poorly controlled,
insulin levels can remain chronically elevated, disrupting hormonal balance. High insulin has been shown to impair egg maturation in women and reduce both sperm count and quality in men. In other words, stable blood sugar isn’t just about energy- it’s about creating the right hormonal environment for conception.
Another major, yet often overlooked, factor is chronic inflammation. Persistent inflammation interferes with hormone signaling, which can lead to irregular ovulation and compromised egg quality. Over time, it may even contribute to structural issues such as uterine scar tissue resulting from chronic pelvic inflammation. For men, chronic inflammation creates a hostile environment for sperm, increasing oxidative stress and impairing healthy sperm development.
Nutrient status is equally essential. Both undernutrition and overnutrition can negatively impact fertility. Undernutrition- often associated with calorie restriction and vitamin deficiencies- is typically more commonly recognized. However, overnutrition- frequently linked to obesity- can coexist with significant micronutrient deficiencies as well. Evaluating and correcting nutrient imbalances is critical not only for conception but also for supporting a healthy pregnancy and baby.
Then there’s gut health, a keystone in hormone balance and nutrient absorption. The gut is far more than just the stomach- it’s an intricate system extending from the mouth to the anus, housing trillions of beneficial bacteria. These microbes play a vital role in extracting, absorbing, and even synthesizing key nutrients. When the gut microbiome is out of balance, nutrient deficiencies and poor digestion often follow. Even more importantly, the gut actively interacts with sex hormones like estrogen, testosterone, and estradiol. When gut function is compromised, hormone imbalances- and fertility challenges- often follow.
By now, a clear theme may be emerging: fertility is deeply interconnected with nearly every aspect of our physiology. This is especially true when it comes to stress. Stress isn’t just an uncomfortable mental state-it triggers real, measurable physiological changes. Chronic stress activates the release of “fight or flight” hormones like cortisol and adrenaline. These can disrupt our overall hormonal balance and negatively affect fertility. Stress can also impair gut health and increase unhealthful coping behaviors such as overeating, excessive alcohol consumption, or smoking-all of which further hinder reproductive health.
To make a long story short, optimizing fertility requires looking beyond hormone labs alone. It means supporting the body as a whole. Balancing blood sugar, calming inflammation, replenishing nutrient stores, healing the gut, and managing stress- so our sex hormones can have the space to do what they need to do.
Can you ovulate and still have hormone dysfunction?

While ovulation is a crucial milestone for fertility, it’s only one piece of a much larger hormonal puzzle. A healthy pregnancy depends not just on releasing an egg, but on creating the ideal environment for that egg to implant and thrive. One of the most critical factors here is the uterine lining. For an embryo to successfully implant, the uterine wall must be thick, nourished, and stable. The hormone responsible for maintaining this environment is progesterone. If progesterone isn’t operating in sufficient amounts, the uterine lining will not be thick enough to sustain a successful implantation.
Timing matters just as much as hormone levels themselves. A well-orchestrated menstrual cycle requires precise communication between hormones. It is critical that the luteal phase, the phase of the menstrual cycle after ovulation, is at least 10 days long. Any time shorter than this is not enough time for progesterone to thicken the uterine wall to sufficient amounts.
Conditions like polycystic ovarian syndrome (PCOS) illustrate this clearly. Some women with PCOS do ovulate regularly, yet continue to experience hormonal imbalance with elevated testosterone levels. Symptoms like acne, excess hair growth, and weight gain can persist despite ovulation, signaling that the underlying hormonal landscape is still out of balance.
The same holds true for thyroid disorders. Both hypothyroidism and hyperthyroidism can disrupt
menstrual cycles and make conception more challenging. And yet, regular ovulation can still occur in both conditions. Once again, ovulation alone doesn’t guarantee optimal fertility.
So in short, Yes- it’s absolutely possible to ovulate and still have hormonal imbalances.
What tests look deeper than standard OB labs?
To gain meaningful insight into fertility, we need to look beyond a single lab panel and take a more
comprehensive, whole-body approach. Utilizing a range of advanced and functional laboratory tests allows us to better understand what’s happening at the microscopic level.
These assessments may include functional blood work, gut testing, mineral analysis, and hormone
metabolism testing. Each test adds another layer of clarity which can help to reveal hidden imbalances that standard testing often misses.
What should I focus on if my labs are “normal”, but I’m not pregnant?
Sometimes all the tests come back “normal”, yet the outcome you’re hoping for still doesn’t happen. If you’ve been there, you know how deeply frustrating- and confusing- that can feel.
When this happens, the next step is often to return to the foundations of health. Supporting fertility starts with making sure your body has enough fuel to run a full, healthy menstrual cycle. That means eating enough- especially the nutrients your hormones rely on to function and communicate effectively.
Nutrition plays a powerful role here. Focusing on gut-supportive foods like fiber-rich beans, whole
grains, and produce. Alongside probiotics like fermented foods can help to nourish the beneficial bacteria within our GI tract. At the same time, reducing artificial sugars supports blood sugar balance and helps to prevent the overgrowth of less-than-healful gut microbes.

Stress management is another key piece of the puzzle. Finding healthy ways to cope during stressful seasons allows your body to spend less time stuck in “fight or flight” mode and more time in a calm, hormonally optimized state. Fertility thrives in an environment of safety and balance.
Finally, this is not a journey meant to be navigated alone. Working with a practitioner who looks at the entire picture, not just a single lab value or isolated symptom, makes all the difference. Fertility is complex, and having someone who understands how all the pieces connect is often the missing link.
Want to learn more?
If you like what you read here, want to know more, but don’t have the time to sit down and read through all our blogs, check out our free private podcast where we break down fertility root causes in more detail. Perfect for those who want to learn more about their hormones and bodies all while still keeping up their busy schedule.
Sources
https://www.stonybrookmedicine.edu/islandfertility/news/sugar
https://rep.bioscientifica.com/view/journals/rep/169/4/REP-24-0197.xml
https://pmc.ncbi.nlm.nih.gov/articles/PMC10097215/
https://azgyn.com/blog/fertility-gut-health
Pregnancy is a season when your body simply needs more—more rest, more support, and yes, more nutrients. During this time, demands for key nutrients like folate, iodine, choline, and vitamin D increase significantly. If these needs aren’t met, deficiencies can have long-term effects not only for you, but for your growing baby as well.
Nourishing your body during this incredibly important and transformative time isn’t optional—it’s foundational to supporting a healthy pregnancy.
Is a healthy diet enough?
Even when you’re eating a well-balanced, nutrient-dense diet, it can still be difficult to meet all of your increased nutrient needs during pregnancy through food alone. This is where a high-quality prenatal vitamin becomes an essential part of your pregnancy toolkit.
Let’s break down a few of the most important nutrients to look for—and why they matter.

Folate
Folate (vitamin B9) is a critical micronutrient for fetal brain and spinal cord development. In the very early weeks of pregnancy—often before someone even knows they’re pregnant—the neural tube forms and closes, eventually developing into the brain and spinal cord. This process typically happens within the first 3–4 weeks of pregnancy.
Folate plays a central role in this process by supporting rapid cell growth and division, as well as methylation—a biochemical process that is essential for proper neural tube closure and healthy brain and spinal cord development.
A quick (and gentle!) biochemistry moment—bear with us. Many supplements and fortified foods use folic acid, which is a synthetic form of vitamin B9. Folic acid must be converted in the body to its active form, methylfolate, before it can be fully utilized. Some individuals have a harder time completing this conversion, which can lead to less-than-optimal absorption.
To bypass this conversion step altogether and support optimal absorption, it’s ideal to choose a prenatal that contains methylfolate rather than folic acid.
Current Recommended Dietary Allowances (RDAs) in the U.S. are:
- 400 mcg/day for women of childbearing age who are not pregnant
- 600 mcg/day for pregnant women
Iodine
Iodine is a crucial micronutrient for thyroid health and function. If you want a deeper dive into iodine’s role in fertility, thyroid health, reproductive health, and hormone balance, be sure to check out our earlier blog: Iodine and Women’s Health: What You Need to Know.
When it comes to pregnancy, iodine deserves special attention. It plays a key role in fetal brain and nervous system development, as well as in thyroid hormone production and regulation for both mom and baby.
The current RDAs in the U.S. are:
- 150 mcg/day for women of childbearing age who are not pregnant
- 220 mcg/day for pregnant women
Because iodine intake varies widely based on diet and food sourcing, it’s an especially important nutrient to confirm is included in your prenatal.

Vitamin D and Calcium
Calcium is essential for bone health, and during pregnancy, needs increase to support fetal skeletal development. At the same time, adequate calcium intake helps protect and maintain mom’s own calcium stores.
During breastfeeding, approximately 3–5% of a mother’s calcium stores can be depleted through breast milk production. While these losses haven’t been directly linked to an increased risk of osteoporosis later in life, ensuring adequate calcium intake before, during, and after pregnancy is still incredibly important.
One of the best ways to support calcium absorption? Vitamin D.
Vitamin D is a fat-soluble vitamin that plays a role in fetal immune system development, overall fetal growth, and—importantly—calcium absorption.
Without getting too deep into the weeds, the active form of vitamin D (calcitriol) helps activate receptors in the intestines that increase the production of calcium-transporting proteins. These proteins work together to improve calcium absorption into the bloodstream—essentially helping your body actually use the calcium you’re consuming.
Current RDAs in the U.S.:
- Calcium: 1000–1300 mg/day (pregnant and non-pregnant women)
- Vitamin D: 15 mcg/day (pregnant and non-pregnant women)
Many perinatal practitioners recommend higher levels of vitamin D for optimal lab levels.
So… which prenatal should I choose?
Understanding nutrient needs is one thing—actually choosing a prenatal is another. With so many options on the market, it’s no wonder this step feels overwhelming.
One important thing to know: many prenatals still rely on outdated RDAs that were originally based on research conducted in men’s bodies—not women’s, and certainly not pregnant women’s.
This is where Needed stands out.
Needed recognized this gap and created prenatals that are science-backed and designed with women’s unique needs in mind—especially during preconception, pregnancy, and postpartum, when nutrient demands are higher across the board.
Needed Prenatal Multi provides 5x more nutrition than outdated RDAs, helping better meet the increased nutrient demands of pregnancy.*
How does Needed compare to other prenatals?

Needed Prenatal Multi Essentials delivers *8x more nutrition than other leading prenatals on the market.
It includes 551 mcg of folate in the methylated form, to support healthy neural tube development and methylation..
And yes—it really is that good.
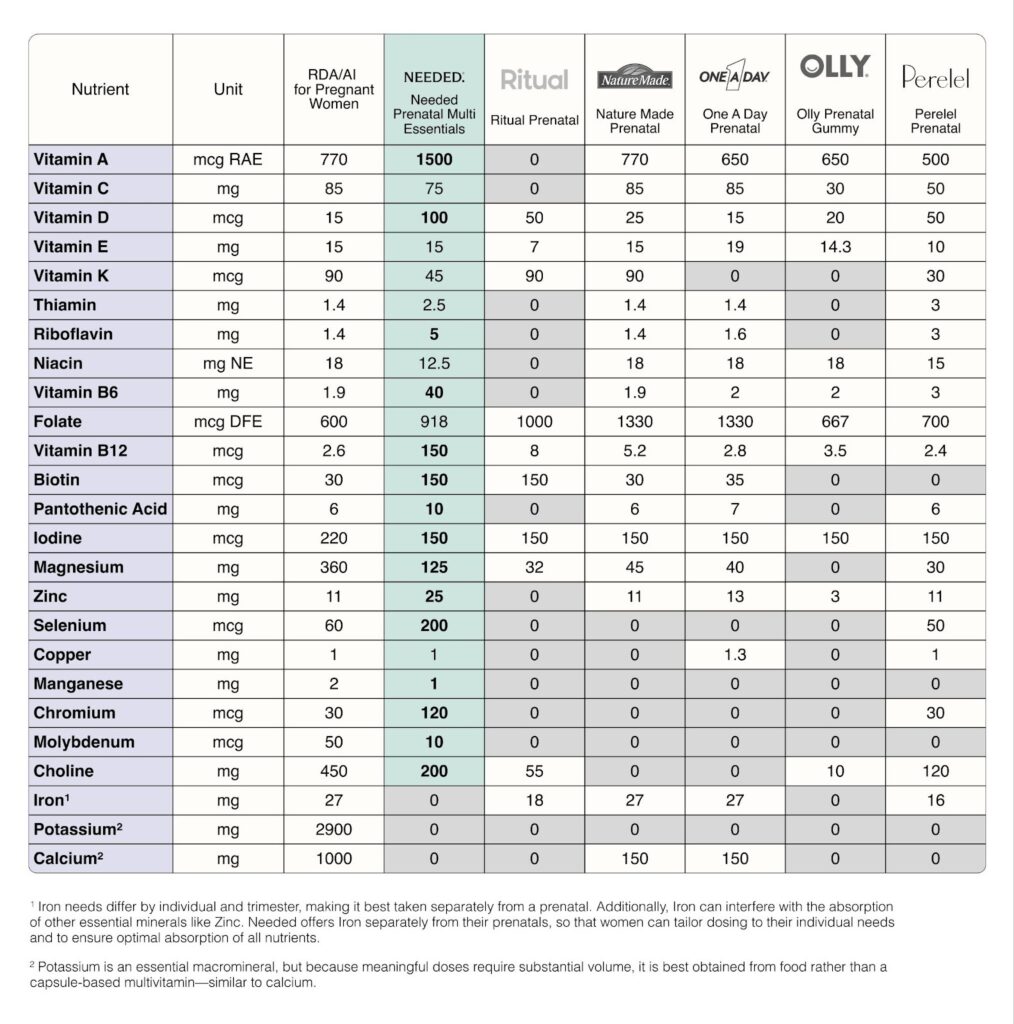
Needed prenatals are third-party tested, meaning an independent, unbiased organization verifies the safety, quality, and accuracy of all label claims. In short: what’s on the label is exactly what’s in the product.
Needed offers multiple prenatal options: capsules and a vanilla powder, so you can choose what works best for you. I used the vanilla powder during my first pregnancy when I simply couldn’t swallow any pills and it was such a game changer for me personally.
You can easily purchase Needed prenatals directly through their website:
https://thisisneeded.com/products/prenatal-multi-essentials
Looking for More Support?
Navigating prenatal nutrition—and figuring out how to best support both you and your baby—can feel confusing. You don’t have to do this alone.
Using every tool available to you, including personalized nutrition guidance and high-quality supplementation, is one of the simplest ways to support a healthy pregnancy. Our 1:1 coaching services are designed to be that extra layer of support—someone firmly in your corner.
Let’s do this together. Reach out today to begin your journey toward nourishing and supporting your growing life with expert guidance every step of the way.
This post is sponsored by Needed, a brand I genuinely recommend to my patients and personally use.
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
*Based on the total daily dosage of nutrients provided compared to leading prenatals as determined by IRI sales data as of December 2025
Sources:
https://ods.od.nih.gov/factsheets/Folate-HealthProfessional/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4933077/
https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/
https://www.niams.nih.gov/health-topics/pregnancy-breastfeeding-and-bone-health

Menopause is often discussed in whispers and framed through negative stereotypes, yet it is one of the most significant and transformative stages of life. Understanding what’s happening in the body—and how to support it through nutrition and lifestyle—can help dismantle stigma and reframe menopause for what it truly is: a period of reflection, strength, and renewed autonomy.
To understand how functional nutrition supports menopause, it helps to briefly revisit how the menstrual cycle works before this transition. While this biology may feel basic, it provides essential context for understanding why symptoms arise and how targeted support can help.

Why Do Hormones Change So Much During Menopause?
Before menopause, the menstrual cycle is regulated by a tightly coordinated hormonal feedback system between the brain and ovaries.
The hypothalamus releases gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones stimulate the ovaries to develop follicles, each containing an immature egg (ova).
As follicles mature, they release estrogen along with inhibin A and inhibin B. These hormones create a negative feedback loop, signaling the brain to slow the release of GnRH, LH, and FSH. After ovulation, the follicle becomes the corpus luteum, which produces progesterone to support the uterine lining. If pregnancy does not occur, progesterone levels fall and menstruation begins.
This predictable hormonal rhythm is what allows for regular cycles—and it’s this system that gradually shifts as menopause approaches.

What Happens to Hormones During Menopause?
Menopause typically begins around age 45, though timing varies widely and there is no “correct” age. Rather than a single event, menopause is a gradual process defined by the STRAW (Stages of Reproductive Aging Workshop) staging model.
Late Reproductive Stage (Stages −3A and −3B)
Cycles are usually regular, and pregnancy is still possible. However, ovarian reserve declines as fewer eggs remain available.
Early Menopause Transition (Stage −2)
This stage marks the beginning of perimenopause. Hormonal signaling from the brain increases, progesterone production becomes less consistent, and menstrual cycles often become unpredictable.
Late Menopause Transition (Stage −1)
Periods become very irregular, with gaps of 60 days or more between cycles. Hormonal fluctuations intensify, often leading to symptoms such as hot flashes, sleep disruption, mood changes, and weight gain. This phase can last up to three years, though duration varies.
Menopause (Stage 0)
Menopause is defined as the final menstrual period.
Early Postmenopause (Stages 1A and 1B)
These stages begin after 12 consecutive months without a period. Hormones continue to stabilize, but symptoms are often most pronounced during this time. Early postmenopause typically lasts two to six years as the endocrine system adjusts to a new baseline.
How Does Functional Nutrition Support Menopause?
Functional nutrition focuses on supporting the body’s changing hormonal, metabolic, and inflammatory needs during menopause rather than simply managing symptoms.
Nutrition for Hormone and Metabolic Health
A Mediterranean-style diet—rich in fruits, vegetables, whole grains, lean protein, and healthy fats—has been shown to reduce inflammation and support cardiovascular and metabolic health during menopause.
Soy-based foods may also help alleviate menopausal symptoms. Soy contains phytoestrogens, plant compounds that interact with estrogen receptors in the body. While phytoestrogens cannot replace estrogen, they can provide mild estrogen-like activity that may help ease symptoms associated with estrogen decline.
Flaxseeds are another valuable dietary tool. Rich in fiber, healthy fats, and lignans, flaxseeds have been shown to reduce the frequency and severity of hot flashes and night sweats. For best results, flaxseeds should be consumed consistently at approximately 2–3 tablespoons per day for at least 12 weeks.
Why Meal Timing Matters in Menopause
When we eat is just as important as what we eat. Late or irregular eating patterns are associated with weight gain and disruption of circadian rhythms that regulate sleep, stress hormones, and appetite. Consuming the majority of daily calories earlier in the day may support improved metabolic health, reduced inflammation, and more restorative sleep.
Movement and Nervous System Support
Regular physical activity—especially walking—has powerful benefits for both physical and mental health during menopause. Walking as little as 12.5 miles per week has been associated with reductions in anxiety and depression, along with improvements in sleep quality and insomnia symptoms.
Can Functional Nutrition Make Menopause Easier?
Menopause doesn’t have to be something you “just get through.” With the right nutritional and lifestyle support, it can be a time of empowerment, clarity, and renewed wellbeing.
Functional nutrition helps identify what your body needs during this transition—whether that’s blood sugar support, inflammation reduction, nutrient repletion, or nervous system regulation.
We’re Here to Support You
Navigating menopause can feel overwhelming, but you don’t have to do it alone. Our 1:1 coaching services provide personalized, functional nutrition support to help you feel informed, confident, and supported through every stage of menopause.
If you’re ready to invest in your health and wellbeing, we’d love to support you. Reach out today to begin your journey.
Sources:
Dr. Haylee Nye, Managing Menopausal Symptoms Naturally: Where to Begin (webinar)
Image Sources:
Organicauthority.com
Freepik.com

Why Routine Blood Work Matters for Women’s Health
Routine blood work is one of the most powerful ways to check in with your body and understand what’s really going on beneath the surface.
Your body can’t exactly tap you on the shoulder and say, “Hey, your vitamin D is low,” or “Your blood sugar is creeping up.” Instead, it communicates through subtle (and sometimes not-so-subtle) signs—fatigue, mood changes, stubborn weight, poor sleep, irregular cycles. While those symptoms are important clues, the most direct way to get answers is through routine blood work.
As a dietitian, I’m a big believer in using data to guide decisions—and I also believe it should be easy and accessible. That’s one of the reasons I personally decided to use Superpower for my own labs.
What Does “Routine Blood Work” Usually Include?
The term routine blood work is broad, but it typically includes several key tests that give a high-level snapshot of your health:
Complete Blood Count (CBC)
A CBC looks at red blood cells, white blood cells, hemoglobin, and platelets. These markers tell us how well your body is transporting oxygen, fighting infections, and clotting blood. Suboptimal levels can point to issues like anemia, inflammation, or underlying infections.
Comprehensive Metabolic Panel (CMP)
A CMP evaluates 14 different markers related to kidney function, liver function, electrolytes, blood sugar, proteins, and acid–base balance. This panel gives valuable insight into digestion, nutrient absorption, mineral status, and overall organ health.
Lipid Panel
This test measures LDL (“bad”) cholesterol, HDL (“good”) cholesterol, VLDL, and triglycerides. These markers reflect long-term dietary patterns, metabolic health, and cardiovascular risk. Elevated triglycerides or LDL can increase the risk of heart disease, while HDL plays a protective role by helping remove excess cholesterol from the bloodstream.
Thyroid Panel
A standard thyroid panel usually includes TSH, T4, and T3. These hormones regulate metabolism, energy, temperature, and growth. Imbalances here can show up as fatigue, weight changes, hair loss, or cycle irregularities—symptoms many women are told are “normal,” but often aren’t.
HbA1c
HbA1c reflects your average blood sugar over the past 2–3 months. It’s one of the most important markers for identifying insulin resistance, prediabetes, and diabetes.
- Below 5.7%: typical
- 5.7–6.4%: prediabetes
- 6.5% or higher: diabetes
My Personal Experience with Superpower
One of the biggest barriers I see—both personally and with clients—is logistics. Scheduling labs, remembering appointments, waiting weeks for results…it’s enough to make routine testing feel overwhelming.
That’s where Superpower really stood out to me.
The sign-up process was incredibly easy, and my blood work came back much faster than I expected. I also loved receiving text updates along the way—no guessing, no wondering when results would arrive.
Once I had my labs, the value really clicked. Having everything clearly laid out made it obvious where things were improving and where I needed support. I could see, for example, that my HbA1c had come down, which was incredibly validating, and that my vitamin D levels were lower than optimal, giving me clear direction on what to address next.
As someone who works with labs every day, I can confidently say: having this kind of insight makes it so much easier to make informed, proactive health decisions instead of guessing.
Making Blood Work Fit Into Your Life
If going to a doctor’s office or lab feels like one more thing on an already full to-do list, Superpower simplifies the process.
Superpower offers blood testing either at home or through one of their 2,000+ partner labs and assesses 100+ biomarkers—far more than what’s typically included in standard annual labs.
Beyond the testing itself, Superpower provides:
- A personalized plan based on your results
- Easy-to-understand data through their member portal
- Ongoing updates as your health evolves
- 24/7 chat access to their team if questions come up
Instead of just handing you numbers and sending you on your way, they help you understand what those numbers actually mean.
The Bottom Line
Routine blood work isn’t about finding something “wrong”—it’s about listening to your body before small imbalances turn into bigger issues. When testing is accessible, clear, and actionable, it becomes one of the most empowering tools for long-term health.
If you’ve been putting off labs because of time, logistics, or confusion around results, Superpower is absolutely worth checking out.
Learn more at: https://superpower.com
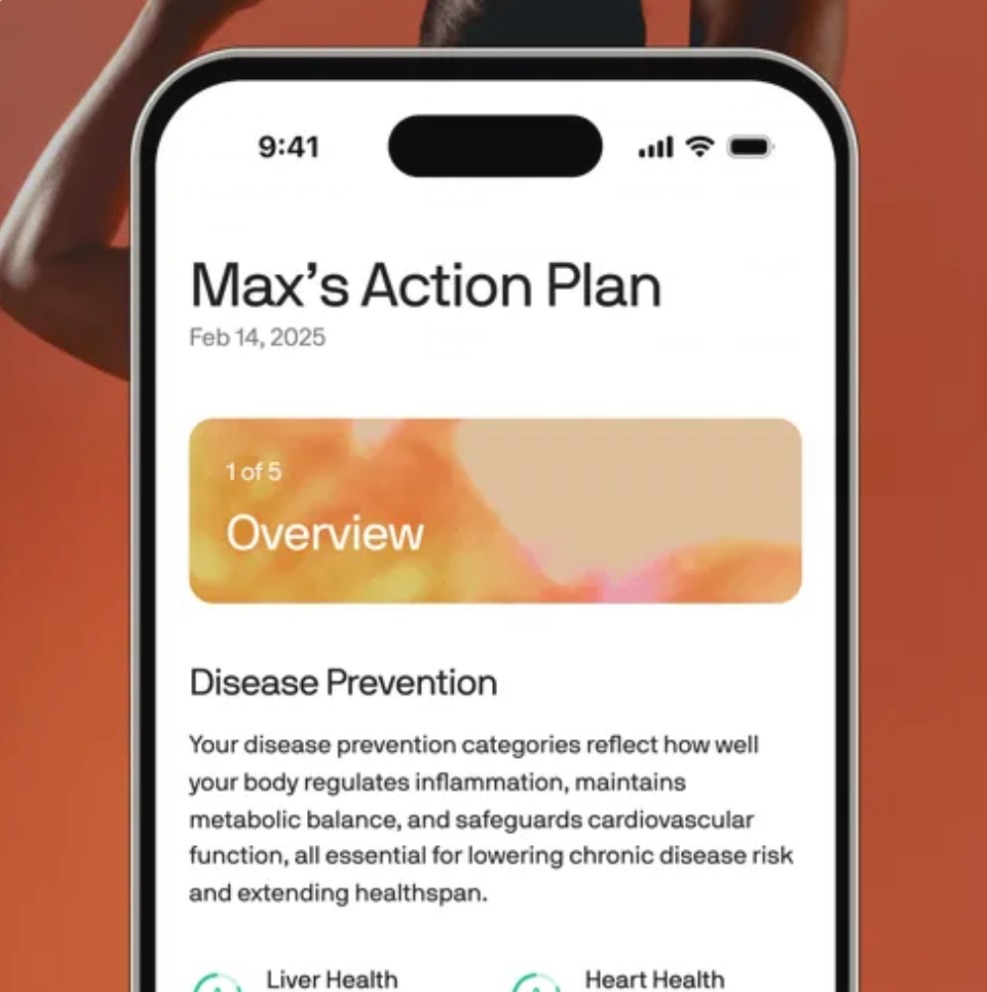
Superhero doesn’t stop there though, based on your bloodwork result a personalized plan is created that evolves with you. All of this data is easy for you to check and access through their website and member portal.
What’s Blocking Your Fertility? Root Cause Quiz Development
Growing my nutrition practice taught me that most women struggling with fertility don’t just need another meal plan or supplement. They need help uncovering the underlying issues that are making conception so difficult. Clients often come to me feeling exhausted, bloated, anxious, or inflamed, yet they can’t connect the dots between these symptoms and their reproductive health. When I discovered Interact, a quiz‑building platform, I realized that an interactive diagnostic quiz could meet people right where they are—online—and guide them toward identifying possible root causes of their fertility challenges.

Interactive quizzes aren’t just fun; they’re powerful marketing tools. The Blogsmith notes that on average a quiz is shared 1,600 times, and in January 2015 nine out of ten of the most‑shared Facebook posts were quizzestheblogsmith.com. 70 % of marketers say interactive content is effective at converting visitors, and 88 % say it differentiates their brandtheblogsmith.com. The average lead‑capture rate for quizzes is 31.6 %, far above the 1–5 % typical for email opt‑instheblogsmith.com. Leveraging these statistics, I set out to build a quiz that wasn’t just entertaining—it needed to deliver meaningful, actionable information while capturing leads for my practice.
The Idea: A Diagnostic Quiz for Fertility Root Causes
My program, The Root Cause Fertility Method, focuses on helping women improve fertility through a holistic lens. Many clients experience sugar cravings, energy crashes, bloating, headaches, acne, insomnia, or chronic stress, yet don’t realize these are often connected to hormonal imbalances, digestive dysfunction, or nutrient deficiencies. I wanted a simple tool to help women start connecting these symptoms to possible underlying causes before they even book a consultation.
Choosing a point‑based system
To do this, I created a 25‑question quiz called “What’s Blocking Your Fertility?” Each question offers two answers—a symptom is either “yes” or “no.” Here’s a sample:
| Symptom category | Sample question | Answer A (points) | Answer B (points) |
|---|---|---|---|
| Blood‑sugar/insulin | Do you experience intense sugar or carb cravings, especially in the afternoon? | “Yep! Feel this all the time” (1 point) | “No, not really” (0 points) |
| Digestion/gut health | Do you often feel bloated even when eating healthy foods? | “Yes, I’m constantly unbuttoning my pants” (1 point) | “No, I rarely feel bloated” (0 points) |
| Inflammation/autoimmunity | Do you feel stiff or achy in the morning? | “Yes, I feel like I’m twenty years older” (1 point) | “No, I’m a spring chicken” (0 points) |
| Nutrient deficiencies | Do you notice brittle nails or hair thinning? | “Yes, I’m constantly finding hair everywhere” (1 point) | “No, my hair and nails are healthy” (0 points) |
| Adrenal/stress | Do you feel wired but tired at night? | “Yes, I’m tired all day and scrolling at night” (1 point) | “No, I have a solid bedtime routine” (0 points) |
Each “yes” answer in a category adds one point to that root‑cause bucket. At the end of the quiz, the category with the highest score indicates the user’s most likely area of imbalance—blood sugar/insulin, digestion/gut health, inflammation/autoimmunity, nutrient deficiencies, or adrenal/stress dysfunction. Every result page offers targeted suggestions (for example, balancing blood sugar with protein and fiber at meals, supporting digestion with probiotics and mindful eating, addressing inflammation through anti‑inflammatory foods, or prioritizing sleep and stress management). This point‑based design makes the quiz feel personalized and diagnostic without overstepping into medical diagnosis.
Building the quiz with Interact
Why Interact?
After researching quiz platforms, I chose Interact because the software is intuitive and flexible. The Blogsmith review highlights that Interact’s user interface is “ridiculously easy to use and navigate,” with a clean design that makes quiz creation straightforward. It allows you to add your branding basics, customize a quiz cover, create result pages, and then jump back and forth between sections as you refine questions (theblogsmith.com). I knew I wanted to design a quiz that looked polished and aligned with my brand, but I also needed the flexibility to adjust questions and scoring logic on the fly.

Customizing my quiz
- Branding and cover – I started by uploading my logo and choosing colors consistent with the Wellspring Nutrition brand. Interact prompts you to set up your quiz cover first, which ensures a cohesive look.
- Result pages – Before drafting questions, I defined five result types corresponding to the root‑cause categories above. Interact lets you add as many result pages as you need and edit them at any time. Each result page includes an explanation of the likely imbalance and a call to action directing readers to schedule a consultation or download a free fertility guide.
- Question & answer creation – Interact allows text‑based or image‑based questions, so I selected images of happy families and healthy food to make the quiz visually appealing. Adding questions is simple: you type your question, write the answer options, and use the points feature to assign values. The platform makes it easy to edit correlations so that one answer can map to multiple results.
- Scoring logic – I enabled the “scored quiz” option. For each answer, I assigned points to the appropriate categories. Interact automatically tallies points as users progress and displays the result page with the highest score when they finish. The platform supports multiple quiz types—including personality, knowledge tests and scored quizzes—so you can choose what fits your goals.
- Lead‑capture form and segmentation – Interact’s integrations with email service providers allow you to add an opt‑in form before revealing results. I connected the quiz to my email service and mapped each result to a segmented list. For example, someone with high blood‑sugar points receives a follow‑up email with tips for balancing insulin and information about my blood‑sugar reset program. Personalized segmentation like this automates nurture sequences without manual tagging.
- Embedding the quiz – Once the quiz was finalized, Interact generated an embed code that I inserted into a dedicated landing page on my website. It also offers a WordPress plugin, but I opted for the code to ensure full control over the page design. I added share buttons because social media is crucial for quiz success.
Following best practices
Interact’s internal data from over 40 k quizzes and 5 million leads has shaped a list of best practices, which was so helpful when creating the quiz. Here are some guidelines I followed:
- Keep it short: Aim for about 2 minutes or 7 questions to maintain engagement. My quiz has 25 questions but each is a quick yes/no, so completion time averages under three minutes.
- Use 3–6 answer options: I limited each question to two choices to reduce decision fatigue
- Offer an opt‑out: I allow users to skip the opt‑in if they just want to see their results, which avoids capturing unqualified leads.
- Call to action: Each result page directs users to book a free discovery call or download my fertility checklist.
Insights from quiz data
In its first month, the quiz attracted seven participants with an 87 % completion rate on early questions. Interestingly, the highest “yes” rates corresponded to symptoms of poor blood‑sugar control: sugar cravings, energy crashes after eating, and waking up between 2–4 a.m. Many respondents also reported digestive issues like bloating and irregular bowel movements, suggesting that gut health is a significant blocker for fertility in my audience. This data is incredibly valuable; it confirms patterns I see in one‑on‑one consultations and helps me tailor my content and offers to address the most common root causes.
The quiz also acts as a conversation starter. Women who score high in the adrenal/stress category often share stories about feeling overwhelmed and emotionally exhausted, and we talk about creating sustainable self‑care routines. Those who score high for nutrient deficiencies are often surprised when we connect brittle nails and hair loss to minerals like iron and magnesium. I always remind users that this quiz is a starting point, not a medical diagnosis. Nevertheless, it invites them into a coaching relationship where we can run functional lab tests and design personalized protocols.
Why interactive quizzes matter
Interactive quizzes drive engagement and segmentation more effectively than static content. Statistics show they convert visitors into leads at a higher rate than traditional email sign‑ups and are widely shared across social platforms. They also help automate personalization; Interact’s integrations let you segment users based on their answers and trigger tailored follow‑up sequences. For practitioners like me, quizzes are not just marketing tools; they’re educational resources that empower people to take the next step on their health journey.
Final thoughts
Creating my root‑cause fertility quiz with Interact was both fun and strategic. The platform’s intuitive interface, customizable design and flexible scoring system allowed me to build a diagnostic‑style quiz that engages visitors and delivers personalized results. The data I’ve collected so far confirms that blood sugar and gut health are the most common blockers for fertility in my audience, which helps me refine my services and content. For example, in my Root Cause Fertility Method program we include a continuous glucose monitor AND the GIMAP stool test because we know that blood sugar and gut health are the top two root causes our audience is working on.
If you’re a health professional or coach looking to generate leads while genuinely serving your audience, I highly recommend experimenting with interactive quizzes. They can be designed for personality‑based insights, knowledge tests, or scored diagnostics, and you’ll gain invaluable insights along the way. To see how my quiz works and discover what could be blocking your fertility, head over to my website and take the quiz yourself! And let me know what you think! 🙂

The Preconception Playbook
This free playbook provides specific actionable tips to get started on your fertility journey, as well as what to avoid while you're trying to conceive.
Get the free playbook